Getting diagnosis right has always been the cornerstone of healthcare: it informs every decision along the patient’s journey, often marking the difference between successful and unsuccessful treatments. But in many ways, the diagnostic process has never been as challenging as it is today. Healthcare providers are overloaded with routine administrative work and struggle with fragmented systems that take their focus away from the patient. On top of that, the total amount of medical data keeps growing – by 48% each year, according to some estimates. While that carries with it the promise of more precise diagnosis and therapy, in reality it often makes it harder to filter out the information that is truly relevant. Clinicians have too much data, and too little time. It’s no wonder professional burnout in healthcare is rampant. According to the World Medical Association, nearly half of the world’s physicians experience symptoms of physical, mental, and emotional exhaustion. A survey that Philips conducted among radiology staff last year confirms that they, too, are experiencing high levels of stress and burnout. And that was before COVID-19 hit. With the added pressure of the pandemic, the need for transformation has become even more urgent. How can we connect disparate workflows to improve efficiency across the diagnostic enterprise? How can we turn information into intelligence? And how do we ensure that patients ultimately benefit in the form of a more precise diagnosis and therapy?
Paving the path to precision diagnosis
Healthcare leaders recognize the need for change. As I detailed in my previous post on digital transformation in healthcare, the COVID-19 crisis is accelerating a shift toward virtual and distributed ways of working on the one hand, and stronger central coordination on the other. Not only will this help diagnostic enterprises weather the current storm – it will also make them more integrated, adaptable, and resilient in the long run.

The truth is: when we critically examined the way we serve our customers at Philips, more than a year ago, we also saw a need for tighter integration of our diagnostic capabilities. For more than a century we’ve been pioneering innovation in medical imaging. But to help address the challenges of today’s diagnostic and clinical service providers, more is needed than a static patient snapshot through high-quality images. Equally important is that we get the right diagnostic insights in the hands of the right people as they build a deeper understanding of the patient over time – enabling them to guide every patient on the most appropriate care pathway. That’s why we decided to pursue even closer integration of our capabilities in diagnostic imaging, digital pathology, and genomics. We’ve also doubled down on our investments in informatics, to help physicians connect information over time and across sites, and in artificial intelligence, to turn that information into actionable insights that support diagnostic decision-making and treatment selection. What unites these efforts is the ambition to advance precision diagnosis in a way that was previously not possible. Together with healthcare providers around the world, we want to bring increased precision to how diagnostic information is acquired, shared, and translated into insights across specialties. These insights then inform clinical decisions – all with the ultimate goal of improving patient outcomes at lower cost, while improving patient and staff experience. What does that mean in practice? Let’s break it down into four areas.
1. Getting diagnostic studies first-time right with smart diagnostic systems
In diagnostic imaging, the need to combine productivity with precision has never been more daunting. Some imaging centers face significant patient backlogs following COVID-19, while new personal protective equipment and disinfection standards add to staff stress. Even under the best of circumstances, unwarranted variation still gets in the way of first-time-right imaging, whether it stems from the specific training and skill level of the technology operator, lack of standardized protocols, or technology that is not well adapted to the unique characteristics of the patient. The result: unnecessary repeat scans that eat up time, budget, and resources, while delaying diagnosis and treatment. How can we help imaging staff get results right the first time? When we probed them for their needs in a survey Philips conducted last year, their answers were revealing: respondents indicated that almost a quarter of their work could be automated, empowering them to do their job with less stress, more efficiency, and more time left to interact with the patient. That’s where smart diagnostic systems come in.

For example, in MR – one of the most complex imaging modalities – we are reducing operator workload by automating exam planning, scanning, and processing. This allows even new operators to proceed with confidence. Similarly, in diagnostic X-ray, technology can support with patient positioning to speed up image acquisition and prevent unnecessary retakes – allowing one clinic to go from scanning 680 patients per month to nearly 1,200 per month. And in ultrasound, arguably the most operator-dependent imaging modality, intelligent new transducers are providing additional support at the point of care to avoid missed findings and enable more precise detection. By adapting technology to the needs of the individual patient, we can further enhance precision in image quality. Take pediatric patients, for example, who range from tiny neonates to overweight adolescents. With an ultrasound solution specifically designed for pediatric assessment, clinicians are able to diagnose pediatric patients more quickly and with more confidence.

We are also helping physicians achieve diagnostic confidence in a single scan by advancing the use of spectral CT, most notably in the diagnosis of cardiovascular and cancer patients. Because spectral CT delivers high diagnostic quality at low contrast dose, it is particularly well suited for examining even the most challenging patients, such as those with reduced renal function who tolerate less contrast agent. One study involving cancer patients with renal insufficiency showed how spectral CT in comparison with non-contrast CT resulted in 34% shorter time to diagnosis and a 25% decrease in unnecessary additional exams, saving $453 on average per additional scan needed. It’s a great example of how smart diagnostic systems can bring more precision that benefits patients and staff alike, while saving costs.
2. Optimizing workflows to drive clinical and operational efficiency
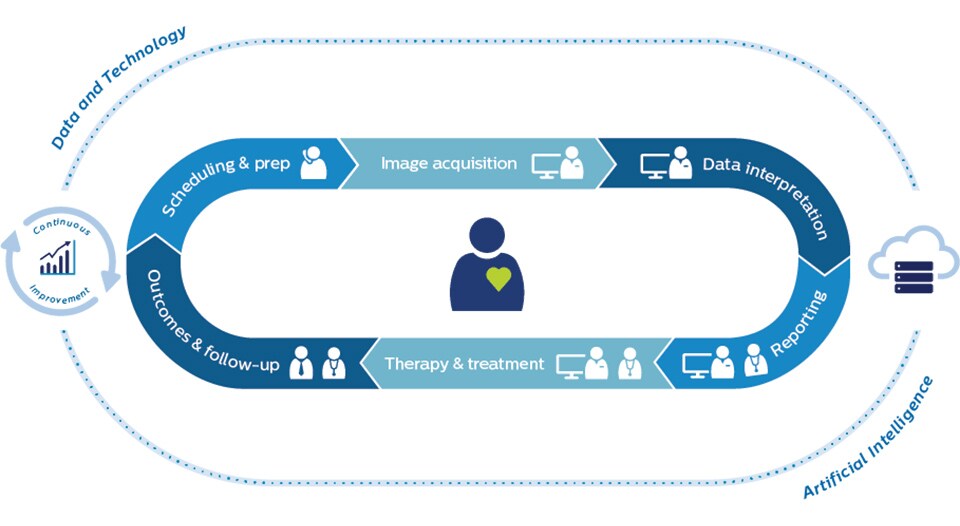
While smart diagnostic technology provides a stepping-stone to precision diagnosis, it’s clearly not enough. In the Philips survey I referred to earlier, imaging staff indicated that workflow-related factors also contribute strongly to getting diagnostic results right the first time – whether it’s patients showing up on time and prepared for their exam, or having easy and complete access to patient information. That’s why we view the diagnostic enterprise as an interconnected system, with the patient at its center. At every moment in the patient’s journey, there’s an opportunity to remove waste and streamline workflows – starting before the patient even arrives at the imaging facility.
Patient no-shows and poor patient preparation have always been a costly disruption to imaging facilities. With the current patient backlogs, financial strain, and patient anxiety resulting from COVID-19, it has become an even bigger priority. Understanding that ‘precision’ starts with proper patient scheduling and preparation, healthcare providers are finding value in remote patient engagement platforms to inform and reassure patients. When we add predictive capabilities to target patients who need extra attention, we are even better able to prevent no-shows. Further along the patient journey, having access to patient information from any location is now more important than ever. Distributed ways of working are quickly becoming the new norm in the wake of COVID-19, with remote image reading creating opportunities to balance workload and leverage specialists across enterprise networks. As distributed ways of working take hold, central coordination is critical. This means we will see a strong rise of clinical and operational command centers – either virtual or physical – that allow for dynamic orchestration of people, data, and technology across the diagnostic enterprise. These command centers will be instrumental in managing complexity and unpredictability. And they will help take the waste out of an already overburdened system.
3. Generating comprehensive patient insights through integrated diagnostics
As physicians amass more and more information about a patient’s condition, how can they make sense of it to get a more comprehensive and accurate view of the patient? The challenge of having too much information is real. That’s why the next frontier for precision diagnosis is integrated diagnostics, which aims to connect the dots across specialties and over time to provide contextually relevant insights at every point in the care journey. It’s a vision we have already started bringing to life. In cancer care, we are supporting multidisciplinary tumor boards with unified patient dashboards that allow the extended clinical team to see all pieces of the patient puzzle in one overview. By automatically pulling together information from disparate sources – including EMRs, lab, pathology, radiology, and genomics data – we can cut down manual preparation time for all involved, and support timely, informed treatment decisions.

In the same spirit of aggregating clinical information, we are helping cardiology teams see the bigger picture in a plethora of patient imaging data, from ECG to echocardiograms and coronary CT. When assessing complex cardiac conditions such as heart failure, overlooking relevant information can lead to preventable patient deterioration. This makes it all the more important that treating physicians have a clear and comprehensive “cockpit view” of a patient at any moment in time. Many opportunities to advance integrated diagnostics remain. For example, as comorbidities are increasingly relevant, we can build stronger bridges between care domains such as oncology and cardiology. Only by seeing patients as a whole person, in the fullness of their clinical and personal history, can we guide and monitor them on a clear care pathway – which brings us to the fourth and final frontier of precision diagnosis.
4. Guiding every patient on a clear care pathway with predictable outcomes
No matter how accurate a patient’s diagnosis, physicians are still left with a formidable challenge: of all the therapy options available, what should be the next step for this particular patient? For highly complex diseases like cancer, that question can be incredibly hard to answer. Every patient is different down to the molecular level, calling for precise and personalized treatment. Yet it’s practically impossible for time-stressed physicians to keep up with every new drug that’s released, every targeted therapy that becomes available, and every scientific study that is published. That’s why we are partnering with leading academic research centers such as Dana-Farber Cancer Institute to make their cutting-edge knowledge more widely available to oncology teams worldwide – helping them select the right care pathway for every patient, based on the unique characteristics of the patient and the treatment options currently available. Through a new partnership with MD Anderson, we are also unlocking the power of genomic markers to personalize cancer treatments and facilitate clinical trial matching. These forays into data-driven therapy guidance hold enormous promise for the future.

Going forward, I envision we will be much better able to predict patient response to a therapy, based on insights lurking in the data of similar patients. It’s a route we’ve already been exploring with our clinical research partners in prostate cancer care. Most therapy options have pros and cons that need to be weighed in an open and informed dialogue between patients and clinicians. This dialogue will benefit tremendously from having evidence-based predictions about survival and recovery rate, but also about quality of life. Once patients are on a clear care pathway, smart and integrated diagnostics supported by efficient workflows remain key to effectively monitor the patient’s condition over time. Whether it’s through multi-modality tumor tracking in cancer patients, or assessing heart function in cardiac patients, the diagnostic journey continues. Because in the end, precision diagnosis is not a static snapshot of a patient: it’s an ever-evolving series of defining moments, with every piece of diagnostic information building on the next, and with every new insight informing the next decision along the patient care pathway. At each of those moments, precision diagnosis allows you to answer with confidence: what should we do next?
Share on social media
Topics
Author

Kees Wesdorp
Former Chief Business Leader Precision Diagnosis Kees Wesdorp led Philips’ Precision Diagnosis business cluster from 2020 to the end of 2022.













