Highlighted products for these procedures

Azurion 7 C20 with FlexMove or FlexArm
As with a mobile C-arm, the FlexMove and FlexArm systems can be brought in from any side of the table for excellent patient access. All movements are fully motorized, and the system can be easily moved in and out without disrupting staff or equipment.

Integrated Getinge Maquet Magnus operating table
Philips Hybrid OR combines the Azurion advanced image-guided therapy system with Getinge’s OR table and more. Benefit from excellent imaging and the flexibility of Azurion seamlessly integrated with the Maquet Magnus table.

Cone-beam CT imaging (SmartCT)
Provides better insights into spinal anatomy to support precise planning and guide effective implant placement.
The Azurion system is the optimal balance between intraoperative image quality and radiation exposure for surgeons and patients."
Dr. P. Scarone
Ente Ospedaliero Cantonale (EOC) Lugano, Switzerland
Customer experiences within Philips Spine suite
Performing minimally invasive spine procedures in the hybrid OR of University Medical Center Schleswig-Holstein (UKSH), Kiel, Germany As physicians perform more minimally invasive spine surgery procedures, many are working in a Hybrid Operating Room (OR). The Orthopedic and Emergency Surgery team at the University Medical Center Schleswig-Holstein (UKSH) explains the benefits they have experienced over the past three years of performing minimally invasive spine surgery in Philips Hybrid OR.
The value of a multi-purpose room In a multi-purpose Hybrid OR more disciplines will benefit from the ability to perform minimally invasive procedures. This reinforces the business case, since costs can be shared and complex procedures can be performed to increase room utilization. All of this supports a high return on investment. The Azurion Hybrid OR offers unique features that create an easy to use and customized OR, for each discipline and procedure from day one.

Spine suite brochure Want to know more about our Spine suite solution?
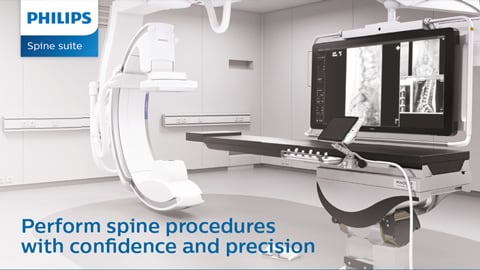
Spine suite results one pager Key benefits of Azurion with FlexMove for spine surgery
Disclaimer Product availability is subject to country regulatory clearance. Please contact your local sales representative to check the availability in your country.