Six impact drivers for sustainable healthcare
Nov 03, 2022 | 9 minute read
Pollution and climate change are threatening the lives and livelihoods of hundreds of millions of people around the world, often hitting the most vulnerable communities especially hard. In his closing remarks, the President of this year’s 77th UN General Assembly, Csaba Kőrösi, said, “Climate change is gradually destroying us… … Yet, some of us still seem not convinced that growing our economies can be balanced with limiting emissions and preserving biodiversity.” According to the US-based CDC (Centers for Disease Control and Prevention), climate impacts such as rising temperatures, extreme weather events and rising CO2 levels affect a wide range of health outcomes.
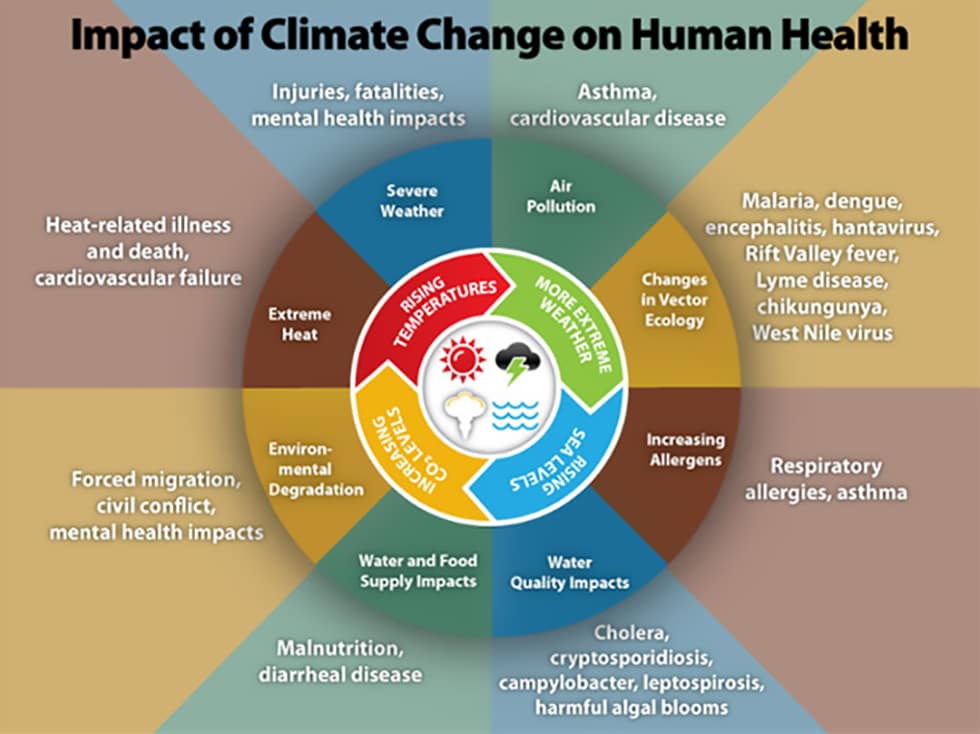
Source: CDC – Centers for Disease Control and Prevention
As far back as 2015, the Lancet Commission stated, “Tackling climate change could be the greatest global health opportunity of the 21st century.” And it still is. Health leaders recognize this potential, as well as the crucial role environmental sustainability plays in achieving long-term population health goals.
Having said that, if healthcare were a country, it would be the world’s fifth-largest emitter of CO2, accounting for over 4% of global emissions [1] – more than the aviation or shipping sectors. This means that, as an industry, we – health technology companies, healthcare systems, suppliers and other stakeholders across the healthcare value chain – have an urgent responsibility to act.
It is time to extend the principle of First, do no harm – the very bedrock of healthcare – to the planet. The good thing is that taking better care of the planet will enable us to take better care of people and so increase our social impact. There is a lot that health technology companies like Philips can do today to help health systems reduce their environmental footprint, integrate sustainable ways of working, and realize the Quadruple Aim of better health outcomes, improved patient and staff experience, and lower cost of care. Not to mention advancing access to care.
So, what are the strategies that health systems can adopt now to help achieve these goals?
1. Reduce direct power consumption – energy efficiency and renewable energy
Hospitals have the highest energy intensity of all publicly funded buildings and emit 2.5 times more greenhouse gas than commercial buildings. [2] At Philips, energy consumption during the customer use phase of our products accounts for around 80% of our total environmental impact. That’s why improving the energy efficiency of our products is a key goal of our EcoDesign program. Our Azurion image-guided therapy platform, for example, offers a 10%-plus reduction in energy consumption over its total life usage, compared to its predecessor [3].
Sustainable user behavior can also make a difference. Healthcare professionals can actively help to reduce the energy consumption of Philips’ MR systems for example, by switching to PowerSave technology when a system is not in use and in between scans.
Philips actively supports a voluntary industry initiative with European trade association COCIR to improve the energy efficiency and material efficiency of medical imaging equipment [4]. As part of the EU Green Public Criteria for medical devices, COCIR has developed methodologies to provide purchasers with all the information they need to calculate running costs and to choose the best equipment for their needs.

For large-scale, energy-intensive operations like hospitals, pivoting to renewable energy can have a major impact. Partnering with like-minded peers can help achieve the necessary scale. Philips, for example, has secured its renewable electricity supply in Europe through consortium-led power purchase agreements. This has been a key factor in Philips being carbon-neutral in its operations since the end of 2020.
For Philips, circularity is a critical step to help our customers create resilient and sustainable healthcare systems. There are several options available to hospitals that can extend the value, capabilities and usability of their existing installed systems. These include adopting ‘as a service’ models, extending lifetime resource efficiency, and implementing smart digital solutions.
2. Reduce indirect emissions through sustainable use of resources and circular economy
Healthcare accounts for 10% of materials used globally every year. [5] Some 40-50% of global CO2 emissions are attributable to materials extraction, supply, and the manufacture of equipment – often referred to as ‘embedded carbon’. Healthcare is a huge consumer of these resources. It is, therefore, crucial that we find ways to use materials for medical systems and devices in a sustainable manner. The noble gas helium, for example, is essential to maintaining the long-term availability of MR scanners, yet its global supply is limited. At Philips, we have developed BlueSeal, a fully sealed magnet that supports the transition to sustainable, helium-free-for-life MR operations, as well as simplifying installation and reducing expensive disruptions to MR services. In contrast to conventional magnet technology, which requires around 1,500 liters of liquid helium for cooling during operation, BlueSeal uses highly efficient, micro-cooling technology, which requires just 7 liters of liquid helium for cooling – less than 0.5% of today’s volume [6].

In many cases, healthcare providers can maximize the return on their initial investments and extend their capabilities through on-site or remote upgrades, instead of having to buy new equipment. Philips SmartPath, for example, gives customers the latest upgrades in workflow, dose management, clinical capabilities and imaging quality on systems they already own. Increasingly, servicing is performed remotely, with AI being applied to support predictive maintenance. This offers customers longer lifetime, increased utilization, and lower environmental impact from their equipment.
Refurbish, re-use, recycle
With healthcare funding under constant pressure, care providers are often looking to expand their resources within a limited budget – but without compromising on quality. As a member of DITTA, Philips is a committed advocate of trade-in and refurbishment of medical imaging equipment. Philips Circular Edition allows customers to benefit from fully refurbished, upgraded and quality-tested technology at lower cost. In this way they can extend the delivery of clinical care while reducing their environmental impact.

If refurbishment is no longer a possibility, we take care of responsible end-of-life management. By recovering valuable parts, we can service older systems, maximizing lifetime value again. If that is also no longer an option, we recycle back to raw materials via local recycling networks. Over 3,000 systems were returned to Philips for responsible repurposing in 2021, as part of our drive to close the loop on all professional equipment by 2025.
3. Implement smart digital solutions
By supporting the creation of virtual resources that deliver maximum value with minimum materials, digital tools and software allow us to ‘dematerialize’. In healthcare, we see this driving a shift from resource-intensive clinical facilities to networked lower-cost settings and the home, thereby expanding access to care.
Today, patients often have to attend multiple appointments for diagnosis, treatment and monitoring. This can involve repeated, sometimes arduous, journeys. The adoption of digital technology and network infrastructure supports prevention and telehealth, or ‘virtual care’, by enabling remote interaction between patients and care givers, thus avoiding the related travel and CO2 emissions.
We also see dematerialization in the form of the transition to cloud-, service- and software-based solutions, which supports savings on the materials required for on-site enterprise hardware and a reduction in CO2 emissions. Studies have shown that power consumption decreases by 84% when customers use large, centralized cloud-based data centers instead of on-premises infrastructure.
Software can also maximize the utilization of hardware. In radiology, for example, Philips PerformanceBridge helps imaging centers get more value out of their systems. This web-based, real-time data platform aggregates data from multiple sources and integrates with the hospital’s image viewer, giving staff the data they need with context. Operational data is clearly presented, making it possible to identify outliers and improvement opportunities, also in energy/material usage.
4. Adopt innovative service models
For our customers and their patients, a system’s functionality and quality of service is what matters, not the system itself. It’s all about being able to offer the best possible imaging and informatics & analytics to support a precision diagnosis and personalized treatment – not a particular piece of equipment. Performance- and access-based models allow care providers to utilize specific functionality as a service. Our Lumify with Reacts portable ultrasound service is a good example. Under this flexible subscription model, users can have access to transducers, an app and online ecosystem, reducing upfront capital expenditure and improving patient access to innovative care.

Similarly, under our Enterprise Monitoring as a Service (EMaaS) partnership with Jackson Health System, Philips retains ownership of the patient monitoring system and is responsible for all hardware, software, and networking upgrades across its network, while the customer pays a per-patient fee.
5. Eliminate waste
Hospitals produce 13 kg of waste per bed per day, of which 15-25% is hazardous waste. [8] Healthcare facilities typically generate a lot of waste, including sharps, trace chemotherapy and pathological waste. Medical consumables are used in massive quantities, and they have a short use life. Consequently, they represent a major source of waste, adding to the financial pressure on health systems. This was exacerbated by the pandemic, which greatly increased the use of medical single-use devices.
At Philips, we aim to design-out waste and pollution and drive the responsible use of resources through our EcoDesign program, which is fully embedded in our innovation processes and drives improvements in four ‘Green Focal Areas’ – energy, substances, packaging, and circularity. For example, we are collaborating with our customers to optimize the lifetime of medical consumables materials and so minimize unnecessary disposal.
6. Buy sustainable and decarbonize the supply chain
The supply chain (scope 3, purchased goods and services) is responsible for 71% of CO2 emissions within the EU. [9] Procurement teams in healthcare have the opportunity to lead and scale change by challenging the way things are done through a sustainability lens, with a focus on value-based rather than cost-based sourcing. More and more, care providers are applying Green Procurement criteria when buying medical equipment, and incorporating minimum standards for sustainability in Request for Proposal (RFPO) or tender procedures. Going forward, it is expected that, in the EU and US, this will increasingly be triggered by Green Procurement standards.

If we are to succeed in decarbonizing healthcare, we need to take an end-to-end view of the value chain. One way health systems can magnify their impact is to select suppliers who have committed to science-based targets for carbon reduction. In 2018, Philips became the first health technology company to have its CO2 emission targets assessed and approved by the Science Based Targets initiative (SBTi). Today, we are going even further, stepping up our supplier sustainability program so that at least 50% of our suppliers (based on spend) will have committed to science-based targets for carbon reduction by 2025. By supporting and incentivizing our suppliers to adopt and meet such targets, we aim to achieve a sevenfold greater impact than simply lowering CO₂ emissions from our own operations.
Time to act!
Leadership commitment to drive change and sustainability across the healthcare value chain – procurement, operations, innovation, service delivery, etc. – is essential if we are to address health systems’ environmental challenges and bring down costs. And it’s not a voluntary 'nice to have': with increasingly stringent environmental legislation on the way in many countries, it makes sense to get ahead of the curve. Setting ambitious targets and committing to report progress on a regular basis are crucial first steps. After that, it’s all about collaborating closely with others in the ecosystem – including care providers, practitioners, knowledge partners and suppliers – to implement change and deliver on commitments.
At Philips, we actively encourage all our value-chain partners to effect sustainable and circular ways of working within their organizations. At the same time, governments can support and stimulate a green approach by setting clear standards, rules and guidelines that apply to all companies, to create a level playing field and drive decarbonization across the board. Businesses need this clarity of purpose. At the same time, investors are demanding an ESG reporting system that enables them to make sound, reliable comparisons and investment decisions.
That’s why we support initiatives such as recently launched by the US Department of Health and Human Services (HHS), in partnership with the White House, to address climate action through the reduction of greenhouse gas emissions. “We have been addressing climate change for many years, teaming up with our partners including our customers and suppliers,” said Robert Metzke, Philips Global Head of Sustainability. “We applaud this new HHS/White House initiative and are confident that this pledge will inspire others to commit to take action against this significant threat.”
We would love to hear from partners intent on driving change and exploring new ways of working to ensure we create a healthcare system that is resilient and future-proof – one that treats more patients more efficiently and in a more sustainable way.
With our collective expertise, innovative capability, and shared awareness of the need to drive change, we can combine sustainable practices with the safe, efficient and effective delivery of care. Now is the time for healthcare providers, health technology companies, governments and other stakeholders to join together and implement the strategies, solutions and services that can deliver more resilient and sustainable healthcare for the generations to come.
Sources [1] Health Care Without Harm (2019). Healthcare’s climate footprint: How the health sector contributes to the global climate crisis and opportunities for action (p.22). https://noharm-global.org/documents/health-care-climate-footprint-report [2] https://www.ecomedsupply.com/Healthcare-Impact-on-Environment-s/1739.htm [3] Compared to predecessor Allura Xper platform; Exact energy reduction depends on configuration [4] https://www.cocir.org/initiatives/ecodesign-initiative/saving-energy.htm l[5] Circular Economy – Circularity Gap Report 2020 https://assets.website-files.com/5e185aa4d27bcf348400ed82/5e26ead616b6d1d157ff4293_20200120%20-%20CGR%20Global%20-%20Report%20web%20single%20page%20-%20210x297mm%20-%20compressed.pdf [6] https://www.philips.com.au/healthcare/resources/landing/the-next-mr-wave/sealed-mr-technology [7] https://aws.amazon.com/about-aws/sustainability/ [8] https://practicegreenhealth.org/topics/waste/waste-0 [9] Health Care Without Harm (2019). Health care’s climate footprint: How the health sector contributes to the global climate crisis and opportunities for action (p.22). https://noharm-global.org/documents/health-care-climate-footprint-report
Share this page with your network







