Developing the cardiac ultrasound technology of the future
Jan 23, 2025 | 4 minute read
Ultrasound is one of the most effective technologies for the diagnosis of various health conditions and their treatment. Portable and relatively inexpensive, it provides the ability to access quality care for huge numbers of people. This is only possible thanks to the hard work and commitment of innovative research and development (R&D) teams.

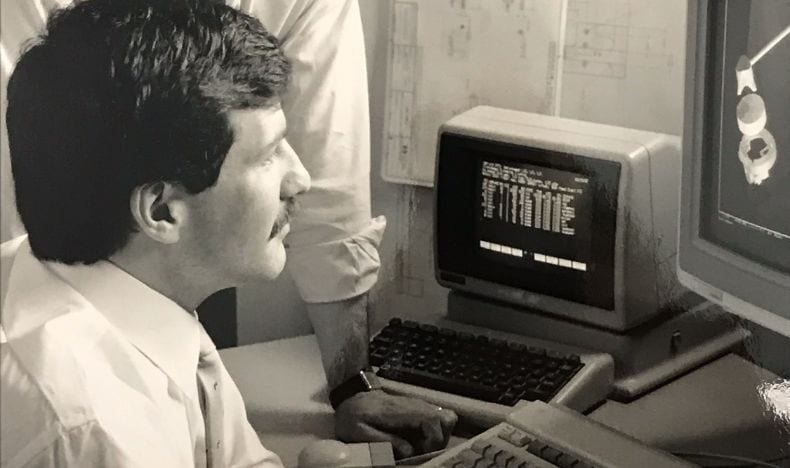
Mike Peszynski, Principal Development Engineer in Transducer R&D at Philips, in Cambridge, Massachusetts, is at the forefront of cardiovascular ultrasound development. Here, he provides an insight into his 37 years of experience and discusses how the ultrasound innovations he and his team have developed are helping to expand access to life-saving care and improve lives worldwide. He also shares his predictions for future ultrasound developments and the role they could play in providing better care for more people.
Using ultrasound to perform “miracles” for patients
The physicians that we work with closely really inspire me. They are the ones who perform miracles with our equipment to help save lives. Hearing a patient’s story of how a product you worked for years to bring to market has positively changed their life… it doesn’t get any better than that!
Developing new-to-world innovative clinical solutions can be very challenging at times, but we work together to bring these complicated concepts into reality and monitor their performance in the field.

The development of ultrasound in the last four decades
When I first started, the ultrasound image was very fuzzy – but even that was a massive step forward for patient safety. Before basic ultrasound scans, checking someone’s heart valve function often meant performing exploratory surgery as diagnostic tools weren’t precise enough. Ultrasound imaging performance has increased dramatically since then. It is also portable, flexible in use, low-cost, and enables high-power imaging.
Ultrasound in interventional cardiology is my passion, and it’s a field in which ultrasound is traditionally used to diagnose organ disease state and cardiovascular function. This area of research provides the kind of technical challenges that have kept my attention throughout my tenure at Philips.
Let’s consider, for instance, the trans-esophageal echocardiogram (TEE) transducer, which is used to scan the heart. Your esophagus is very close to the back of your heart, and the closer we can get to the heart – and the less separation between it and the transducer – the higher frequency ultrasound we can use, and therefore the higher quality images we can achieve. From an engineering perspective, developing a small and efficient enough transducer to provide real-time 3D images of your heart from the esophagus is extremely challenging.
Now imagine taking this device and miniaturizing it again, enabling it to safely fit inside the chambers of your heart for an even higher resolution view of cardiac structure and function. A new Philips’ miniaturized intracardiac transducer enables just this, benefiting patients by enabling access to certain structural heart disease and electrophysiology procedures that otherwise might not be possible.

Supporting access to care for the critically ill and underserved communities
The two main groups for whom our innovations are expanding access to care are critically ill patients who don’t meet previous safe selection guidelines, and those in underserved communities without access to basic medical care. Advances in sophisticated technology mean a new mini 3D transducer has almost identical imaging performance to an adult TEE but in a smaller size, enabling access to real-time 3D imaging for pediatric patients as small as 5 kilograms. This includes complex congenital pediatric cardiac cases as well as those who cannot tolerate the anesthesia required for the larger probe. For pediatric patients, you might help extend their life by maybe fifty or sixty years – far more than in adult disease management, which is amazing.
In underserved communities that lack the resources to transport patients to medical centers, access gaps can be bridged with ultrasound handheld devices that are low-cost to purchase and easy to learn and use.

What does the future look like for ultrasound research
The future looks bright! The promise is twofold: firstly, image precision will continue to improve through developments in transducer architectures and ultrasound system algorithms. Continued improvements in both areas are required to optimize all the artificial intelligence (AI)-based solutions that we've been talking about.
Secondly, miniaturization is going to continue making this technology even more accessible and convenient. Based on the combination of high imaging precision in a low-cost handheld device, enhanced with AI-driven diagnostic algorithms, I can imagine a future where ultrasound becomes accessible almost anywhere – even beyond clinical settings.
Once that becomes possible, it will be a huge area of expansion that would support better care for even more people, for generations to come.









