The four pillars of a value-based healthcare future

Get the latest Philips Future Health Index news in your mailbox

Jan 26, 2018 - reading time 4 mins
By the FHI editorial team The Philips Future Health Index editorial team is always on the look-out for great content pieces that discuss the future of health, selecting the most interesting health-related stories for you to read.


Increasing the cost of healthcare isn’t sustainable, but we can improve the outcomes for the money spent. The World Economic Forum is working towards building a framework for value-based healthcare, yet this is still proving difficult to implement at sufficient speed and on a global scale. Many organizations have institutionalized the value-based model, but there are still no significant examples of entire national health systems doing so. The real potential of the model will be realized only when the approach is applied successfully at scale – at the regional, national or international levels. As part of the movement to make value-based care a reality, WEF has developed four key pillars of a shift towards this more patient-centric approach:
Data and health informatics
Value-based healthcare demands a comprehensive informatics infrastructure for collecting, sharing and analyzing data information for each population segment along the full cycle of care. Health informatics systems need to share common data standards and architecture to be most effective, but uptake and use remain inconsistent in both developed and developing markets. With 75% of HCPs willing to share health information about a patient with other HCPs, the industry needs to harness this willingness and co-create more effective systems that can produce better outcomes.
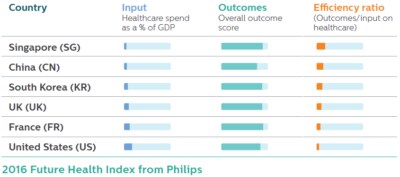
Benchmarking, research, and tools
Only highly granular levels of data about health outcomes can help identify best practice treatments more easily and dramatically reduce inefficiency. This level of detail requires systemic benchmarking, new types of research and the development of sophisticated decision-support tools. Emerging markets tend to lead the way in terms of achieving positive outcomes relative to the investment made into the health system, while developed markets showed more excessive funding (as a proportion of GP), without achieving similar or proportionate outcomes. Older ‘legacy’ health systems can look to the emerging markets for guidance on how to achieve greater parity between healthcare spending and outcomes.
Measurement is the first step but needs to be considered in the sense of benchmarking and then change protocols. We need to ‘measure, benchmark, improve, measure, benchmark’ … better systems need to be better unified and aligned with all stakeholders around the outcome of good care.
Arnaud Bernaert
Head of Global Health and Healthcare Industries , Member of the Executive Committee, World Economic Forum
Delivery organizations and change management
Most provider networks are currently organized around function at each stage of the care chain – but this makes it difficult to achieve true transparency and effective coordination. In theory, this should allow patients to find the most appropriate treatment setting for their condition, but in practice, this often means each link in the chain is managed separately. As a result, incentives for clinicians at the various levels often conflict. Sweden’s healthcare, for example, is based on hierarchy and not demand. All patients, no matter their background and status, proceed through the system in the same way, eventually coming to a place where they receive the right diagnosis and treatment.
Incentives and payments
Many remuneration models in the private sector simply reward providers for the volume of treatment they provide, meaning it can be more profitable to prolong illness than treat it. In the public sector, the fragmentation of priorities and objectives across government agencies can lead to compartmentalized spending, rather than a holistic approach. At a global level, could an overall shift to incentivizing prevention be more valuable in the long term than focusing on treatment in the here and now?
Cleveland Clinic (CC) strives to keep all its patients - including its own employees - healthy. Employees and their spouses who are enrolled in the employee health insurance plan can earn up to 30% off thier insurance premiums. To attain the incentives, those with a range of chronic conditions can enroll in programs that help them meet personalized medical or nutritional goals. These programs have helped CC keep premiums down and encourage patients to stay healthy and be in control of their wellbeing. In 2016, CC managed to reverse annual healthcare cost increases and saw a decline in spending at a rate of about 2%.
Areas for accelerated progress
WEF has identified the following areas that can change relatively quickly and have a real impact on our four pillars and the move towards value-based care:

