Trust at the heart: shaping the future of cardiac care with people-centered AI
Aug 27, 2025 | 3 minute read
Heart health is central to our well-being, yet cardiovascular disease affects 1 in 12 people globally [1], with patient numbers rising in both volume and complexity. This presents not just a challenge, but also a powerful opportunity: by harnessing the potential of digital technology – and AI in particular – to enable earlier diagnosis, more personalized care, and more efficient workflows, we can make high-quality cardiac care more widely accessible. The key to making this work? Building trust in AI that puts patients and professionals first.

Speaking with colleagues in cardiac care worldwide, I see firsthand the increasing workload and complexities they face across both outpatient consultations and procedural care. Each day, they navigate fragmented systems and burdensome documentation. This takes time away from connecting with patients, which is the main reason many of them entered medicine. In fact, recent data from our Future Health Index survey show that 79% of cardiac care professionals report losing clinical time due to incomplete or inaccessible patient information, with nearly half of these losing more than 45 minutes each shift. Combined with ongoing clinician shortages in cardiac care and rising demand from aging populations, these challenges place enormous pressure on professionals, contributing to increasing burnout rates. Patients are also affected, facing growing delays in accessing cardiac care. Our Future Health Index data underscores this issue, showing that globally, nine out of 10 cardiac patients experience significant delays, waiting nearly 12 weeks on average to see a specialist. Those delays come at a real human cost: almost one in three cardiac patients reported that their condition worsened during their wait to see a doctor, resulting in hospital admission.
How AI can help – and why trust matters
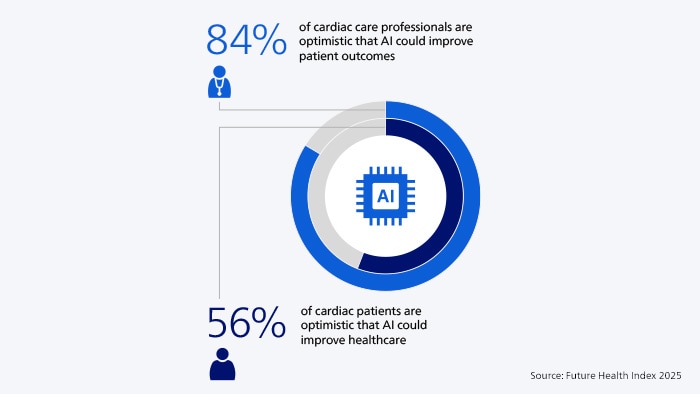
Although cardiac care faces challenges, AI offers promising solutions. According to our survey, most cardiac care professionals believe AI can free up time for better patient care. Over 80% say AI can automate repetitive tasks and extend capacity to treat more patients. What’s more, 83% believe that AI and predictive analytics could save lives by enabling early interventions. Already today, we’re seeing how AI can play a role in supporting more proactive and preventive care by identifying early indicators of heart failure during routine ECG examinations. But a challenge remains. Our findings reveal a major gap in perceptions around AI: while 84% of professionals believe AI can improve patient outcomes, only 56% of patients share that optimism. That’s a significant gap – and one that clearly indicates the need to build greater trust and transparency around AI. Patients worry that relying more on technology means less face time with their doctor. Cardiac care professionals have their own concerns as well, most notably around legal liability and the need for AI systems to be carefully monitored and evaluated. This aligns closely with what I’m hearing from healthcare leaders: they’re betting big on an AI-enabled future – but they want clear assurances to go with it. And the onus is on all of us, including industry, to get this right.
Building patient trust in AI
So how can we build that all-important trust in AI, to ensure AI delivers on its full promise of helping provide better care for more people? Our Future Health Index offers vital clues, all pointing to the need for a people-centered approach to AI innovation that puts patients and professionals first. Cardiac patients are clear about what would build trust: more than anything else, they want to hear about AI from the people they place their confidence in – their doctors, nurses, and healthcare systems. This finding mirrors a 2024 Gallup poll, which found that despite a general decline in public trust, healthcare professionals remain among the most trusted professions. Above all, patients want to feel heard and understood. Building trust means offering clear, accessible explanations about how AI is used, what benefits it brings, and – where possible – giving patients choices in how it’s applied. For example, in digital triage systems, patients could be given the option to have their symptoms assessed through an AI-powered e-consult for faster guidance or wait for a traditional in-person consultation if they prefer. Some may value the speed and convenience of digital triage, while others feel more comfortable speaking with a clinician. Giving patients that choice reinforces trust and ensures AI supports care, rather than replacing the human connection at its heart.

Designing AI that works for clinicians
And what about cardiac care professionals themselves? How do we earn their trust in AI? This is where our survey also offers valuable insights. Unsurprisingly, professionals want to know who’s accountable when AI gets it wrong. They also seek clear guidelines for its use, insight into its limitations and scientific evidence of its effectiveness. Again, this aligns with what I’m hearing from customers – many are looking for clarity on how an AI solution performs for their specific patient population. What’s striking is that, despite 75% of cardiac care professionals being involved in the development of new technologies, only 36% feel those tools are designed with their needs in mind. To me, the takeaway is clear: we need to do an even better job of co-creating AI tools with clinicians – to build solutions that are genuinely helpful, support their workflows and enhance their expertise. I also see a critical role for technology providers like Philips in delivering AI through integrated platforms, rather than contributing to a proliferation of point solutions that only add complexity.
Trust begins with transparency
In all of this, I believe transparency is key. Not only in clarifying what AI can and cannot do today, but also in explaining how the AI was trained and identifying where further validation is needed as we scale these solutions to reach more patients. When we lead with transparency, we create the confidence – not just for patients and professionals, but for all stakeholders, including regulators, policymakers and technology providers – to engage, collaborate and evolve together. I invite you to explore the 2025 Future Health Index cardiology snapshot for a full view of how AI is shaping the future of cardiac care, and how we can put patients and professionals at the center of it. Though technology is rapidly advancing, its real value lies in how it supports caregivers and patients alike. With effective use of AI, we can keep their relationships at the heart of healthcare, and deliver more timely, high-quality care for people with cardiac conditions.
Share this page with your network








