Co-creating AI solutions that free up time to spend with patients
By Philips editorial team ∙ Jul 11, 2025 ∙ 3 min read
Imagine a radiology department with over one hundred staff members analyzing thousands of CT images daily. Every minute of efficiency gain and workflow improvement means radiologists can spend more time with patients. Several years back, the radiology department at the Hospices Civils de Lyon (HCL) in France began a research collaboration journey with Philips to advance task automation using AI. Many of the algorithms generated in this clinical partnership are now available to radiologists everywhere via Advanced Visualization Workspace.
Case study at a glance

“Our initial need was very clear,” says Loïc Boussel, Professor of Radiology at Hospices Civils de Lyon (HCL) and Head of the Radiology Department at the Hôpital de la Croix-Rousse, one of the main hospitals in Lyon, France. “We needed to free up time to spend with patients. Every minute of drawing circles on images is a minute that cannot be spent talking to a patient, explaining their medical condition, or answering questions.”
Dose reduction with CT classification
In 2018, HCL and Philips started to explore the opportunities of AI. The first step was the classification of CT images. Professor Boussel: “We perform many chest CT scans in the hospital. Most patients only need a scan of a specific body area: the neck, thorax, or abdominal. The more specific we can target, the better we are able to minimize the X-ray dose. In our first study, we developed an algorithm to classify the thorax, abdominal, or neck during a thoracic CT scan. This method has helped us raise awareness among radiology technicians to limit exploration to the region of interest only. Reducing the margin could reduce the X-ray dose on average by 20 per cent. That is quite impressive for an algorithm that only took a few months to develop.”
We needed to free up time to spend with patients. Every minute of drawing circles on images is a minute that cannot be spent talking to a patient, explaining their medical condition, or answering questions.

From emphysema to COVID-19
The research soon shifted from classification to segmentation. “For patients with emphysema, we need to determine the percentage of the lung affected,” says the radiology professor. “Together with Philips, we developed an application to segment the lungs and calculate the percentage of emphysema. Just when we had developed the first version of the system, the COVID-19 pandemic spread. We used our segmentation model in addition with a dedicated lung parenchyma analysis module to calculate the percentage of lesions on a lung of a COVID patient. This percentage was an important indicator for patient follow-up.”
From one day per patient to only seconds
AI not only supports clinical decision-making but also saves radiologists in Lyon time – as was the initial objective. “Patients with pulmonary fibrosis, which is a severe lung disease, need to be closely monitored to see how quickly the lung deteriorates. The progression pace determines the type of therapy a patient needs. Using AI, we can now quantify the decay of the lung in a matter of seconds. By hand, it takes several hours per patient.”
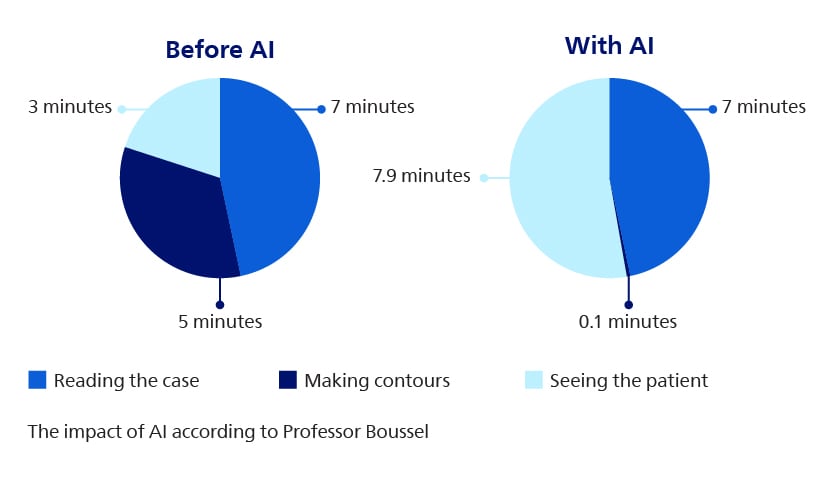
Even when efficiency gains are smaller, the impact should be tremendous; he adds: “For example, a radiologist has on average fifteen minutes to spend on a cardiac case. Before AI, I used to spend seven minutes reading the case, five minutes making contours, and the rest of the time, which was three minutes, seeing the patient. With AI, those five minutes are reduced to a few seconds. This means we can spend over twice as much time with our patients, discussing the outcome, answering questions, and offering explanations.”
Working backward from a need
The radiologist and his team always start with improving clinical outcomes as the starting point for every research project. “We don’t want to develop a tool just for the sake of having a tool. You always start with the clinical need. We also spend time thinking about how to integrate the algorithm into the software and how we should display the results in a way that is convenient for the radiologist. Together with the Philips team, we really think about how to deal with certain problems and which paths we should follow to answer these questions. For me as a researcher, but also for our two PhD students, it is very interesting to combine hospital and industry perspectives.”
Two PhD students, two Philips researchers and an innovation account manager of Philips are working on-site in Lyon. According to the head of the radiology department, this is a game-changer: “ It speeds things up. You meet, have lunch, and discuss your latest results or ideas. That creates great dynamics and strengthens collaboration.”
Ambitions
HCL and Philips still have many ambitions together. “Recently, we developed a system to segment the abdominal aneurysm. Our idea is to see whether we can use the shape and composition of aneurysm to predict how the aneurysm is going to grow and when the patient will need surgery. To do this, we need to segment the whole aorta and the whole aneurysm.”
“One of the great things about developing models with Philips is to see your final product being used at the clinic. You don’t notice AI in the segmentation and image reconstruction in Advanced Visualization Workspace. As a user, you simply see a tool that segments faster and with better results.”
Before AI, I used to spend seven minutes reading the case, five minutes making contours, and the rest of the time, which was three minutes, seeing the patient. With AI, those five minutes are reduced to a few seconds. This means we can spend over twice as much time with our patients.
Disclaimer: Some of the features and applications described reflect investigational research and are not commercially available or cleared for clinical use. Product availability and regulatory status may vary by country. Please consult your Philips representative for details specific to your region and product configuration.







