This article was co-authored by Jan Kimpen, Chief Medical Officer at Philips and Ruben Osnabrugge, Global Strategic Program Lead Value-based care at Philips. What is the effect of the COVID-19 pandemic on the transformation of healthcare systems around the world? Will the increased adoption of virtual care technologies, interoperable data platforms and standardized outcome measurement be the accelerator we need for value-based care? Or does the financial impact of the pandemic force hospitals and medical staff to fall back to short-term revenue generation under the traditional fee-for-service model?
An update on value-based care in 2020
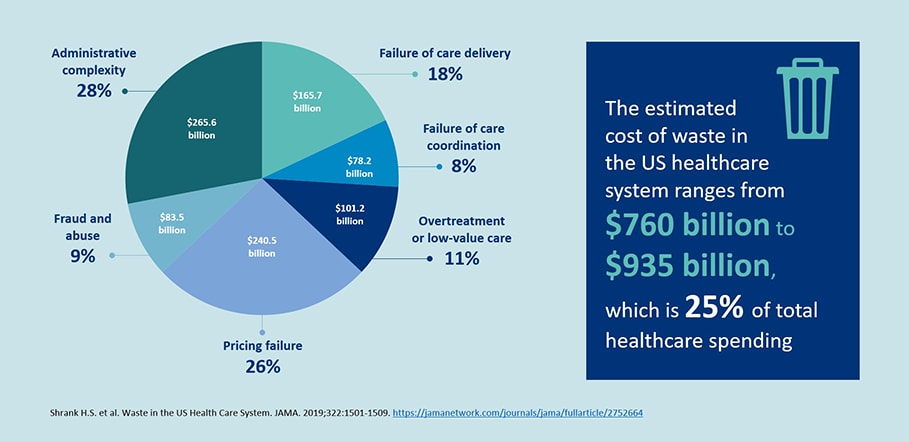
Healthcare costs keep on rising across the globe and increasingly threaten other parts of the economy. Even without a crisis, close to $1 trillion, or 25% of total healthcare spending, is spent each year in the US alone on non-value adding aspects in the healthcare system and can be considered waste [1]. These are truly staggering numbers - can you imagine how much we could achieve if these resources weren’t wasted but rather invested in better patient outcomes?
Value-based care (VBC) models have been developed to address these challenges. In these models, providers are reimbursed based on quality (or value) metrics as opposed to the quantity (or volume) of services delivered. Healthcare providers and payers are working together to design new patient-centric care delivery and payment models that reduce fragmentation and discontinuity and incentivize seamless and integrated care along the patient journey. There is an emphasis on reducing costs and improving outcomes that matter to the patient. Industry has to fall in line with this transformation in healthcare. At Philips, we enable VBC outcomes with our health system customers and partners by helping them achieve the Quadruple Aim, together. Since we are active across the care continuum, from personal health to connected care, and from precision diagnosis to image-guided therapy, we aim for actionable insights to steer towards better outcomes and improved patient and staff experience, while reducing the cost of care. To learn more, you can download our position paper on implementing value-based care here. The path towards VBC has been long and over the years the percentage of total US healthcare payment that is tied to alternative payment models has now risen to 36% [2]. Further adoption is hampered by complex and conflicting interests and structures in the industry as well as IT infrastructural challenges and ever-increasing administrative complexity. VBC training and education should also be taken into account more - more than three-quarter of younger healthcare professionals have very little knowledge about value-based care or only knew it by name or even knew nothing at all, as indicated by results from our latest Future Health Index survey [3].

Impact of COVID-19 on value-based care
While the coronavirus threatens the lives of many across the globe, the economic consequences are also enormous. Even before COVID-19, healthcare expenditure in the US was expected to rise at a 5.4% per annum and at this pace would reach $6.2 trillion by 2028 [4]. This corresponds to almost 20% of the gross domestic product (GDP). Once we get back to a new normal in healthcare, it is expected that healthcare payers (government, private payers and employers) will again aggressively try to reduce healthcare spending, with a focus on innovative payment models. We expect both a short-term and long-term effect of the current COVID-19 crisis on value-based care.
Short-term effect: Slowdown of value-based payment models to get through the crisis
All types of VBC arrangements, including bundled payments, capitation models or pay-for-performance, require some form of capital commitment to take on the inherit risks of these payment models. However, many healthcare providers are struggling with their revenues under COVID-19 and the American Hospital Association estimated that the total four-month financial impact on America’s hospitals will be more than $200 billion [5]. With this significant impact on top of existing balance sheet constraints, it is uncertain whether healthcare providers will continue their pursuit of risk-based contracts with payers. Providers struggling to make up losses endured during the outbreak may be even more reluctant to take on upfront financial risk in the short term. They might focus more on short-term revenues and become more risk averse. Indeed, a survey among 226 accountable care organizations (ACOs) shows that almost 60% are likely to quit their value-based contracting [6]. There are signs of the US government working to sustain the adoption of VBC models. The Centers for Medicare and Medicaid Services (CMS) has been providing relief to providers by making temporary exceptions to the quality reporting programs and value-based purchasing programs [7]. This reduces their reporting burden and softens the downside of being in risk-sharing agreements. Moreover, the launch of a new ACO model is postponed, which shows the commitment of CMS to be a good partner for value-based care providers [8].
With strong value-based, population health management networks, providers become more resilient and more adaptable to potential future crises.
Longer-term effect: COVID-19 showed that value-based delivery networks are the way forward
Despite these short-term considerations, value-based care models continue to be critical in achieving the Quadruple Aim. The response of CMS to sustain value-based care initiatives is reassuring. Further, the pandemic in fact re-emphasizes the importance of implementing value-based delivery models. The COVID-19 crisis is hitting hardest among individuals with poorly managed chronic conditions, including COPD, cardiovascular disease, obesity and diabetes. These conditions are closely related to social determinants of health (i.e. the conditions in which people grow, live, work and age) [9]. Too many people with chronic conditions have been left vulnerable and the need to manage their conditions has never been clearer. Managing these populations heavily relies on good primary care, telehealth, remote patient monitoring and digital health education. These are exactly the aspects that need to be accelerated to make value-based care a reality [10]. That’s why Philips recently joined forces with the American Telemedicine Association (ATA) to help further the adoption of telehealth across the industry, demonstrating its commitment to connecting care across acute, post-acute and home care settings [11].

With the current crisis speeding up the acceptance of telehealth and connected care, which are pivotal technologies in the transformation of healthcare [12], the future of value-based care can be even brighter than before the crisis. Moreover, when strong value-based, population health management networks are in place, providers become more resilient and more adaptable to potential future crises. This is illustrated by Oak Street Health, a network of primary care centers in the US providing high-touch value-based care for Medicare beneficiaries [13]. This network, serving 80,000 adults from diverse backgrounds across eight states, already had a strong remote care model in place. Their platforms have swiftly adapted to the COVID-19 situation and include social determinants support. Not only was there ample support for wellness checks and hospital-like care experiences at home, but also additional services like grocery delivery and trying to reach individuals with limited internet connection were applied. Oak Street Health did not wait for what is reimbursable, but focused on what they were already doing for their patients: providing longitudinal, primary care, easily accessible from the safety of their homes.
The future of value-based care can be even brighter than before the crisis.
And there are other examples, for example in the Netherlands, where we launched a national online portal that allows Dutch hospitals to seamlessly share COVID-19 patient data with one another, in response to the immediate need for seamless, secure sharing of medical information, while safeguarding patient privacy. Since its launch on March 28, 95% of Dutch hospitals have used this portal [14]. At Philips, we are committed to the transformation towards value-based care. Not only by providing ventilators, but also with telehealth solutions and smart biosensor technologies, supporting caregivers and patients across the health continuum, all building on interoperable digital platforms [15, 16]. When these technology-enabled population health strategies are put in place across the globe, healthcare systems will be better prepared for creating optimal value of care, in everyday practice and in times of crisis. [1] Shrank H.S. et al. Waste in the US Health Care System. JAMA. 2019;322:1501-1509. https://jamanetwork.com/journals/jama/fullarticle/2752664 [2] Health Care Payment Learning & Action Network. Measuring Progress: Adoption of Alternative Payment Models in Commercial, Medicaid, Medicare Advantage, and Traditional Medicare Programs. October 24, 2019 [3] https://www.philips.com/a-w/about/news/future-health-index/reports/2020/the-age-of-opportunity [8] https://www.cms.gov/files/document/covid-innovation-model-flexibilities.pdf [9] https://www.who.int/social_determinants/sdh_definition/en/ [13] https://catalyst.nejm.org/doi/full/10.1056/CAT.20.0148

Share on social media
Topics
Authors

Jan Kimpen
Chief Medical Officer, Royal Philips Before joining Philips in 2016, Jan Kimpen, Professor of Pediatrics, was CEO of the University Medical Center in Utrecht. He leads the global clinical team of Philips, focusing on advocacy, customer partnerships, clinical research and medical consulting, and is responsible for the annual publication of the Philips Future Health Index. He is a strategic advisor for commercial and clinical strategy, market reimbursement, R&D roadmaps and partnerships and M&A, and provides thought leadership on relevant clinical and medical topics. Jan participates in the WEF Global Future Council on Healthcare, the American Heart Association alliance and the Board of Sanara Ventures in Israel. Jan is president of COCIR, the European trade union for imaging, healthcare informatics and radiotherapy.
Follow me on

Ruben Osnabrugge
Global Strategic Program Lead Value-based care Dr. Osnabrugge is currently the Global Strategic Program Lead Value Based Care at Philips. Prior to this he was a Cardio-Thoracic Surgeon with special interest in Interventional cardiology (structural heart) at the Erasmus MC, Rotterdam. His Ph.D. thesis was “Costs, Quality and Value in Cardiovascular interventions: Implications for clinical decision-making”, for which he spent a Fullbright Scholarship at the Mid-America Heart Institute in Kansas City. He performed cost-effectiveness and quality-of-life studies of major interventional cardiology trials, co-authored >45 peer-reviewed medical articles in top peer-reviewed medical journals, contributed to European clinical guidelines and was faculty at the major cardiovascular professional organizations EuroPCR and the European Association of CardioThoracic Surgery (EACTS). Apart from his medical degrees, he holds a Master of Science degree in Clinical Epidemiology from the Netherlands Institute for Health Sciences (NIHES) and Harvard School of Public Health, Boston MA., as well as a degree in Health Economics, from Erasmus University Rotterdam.
Follow me on




