Mar 17, 2019
DEFINE PCI study finds treatable cause for significant rates of residual ischemia in coronary stent patients
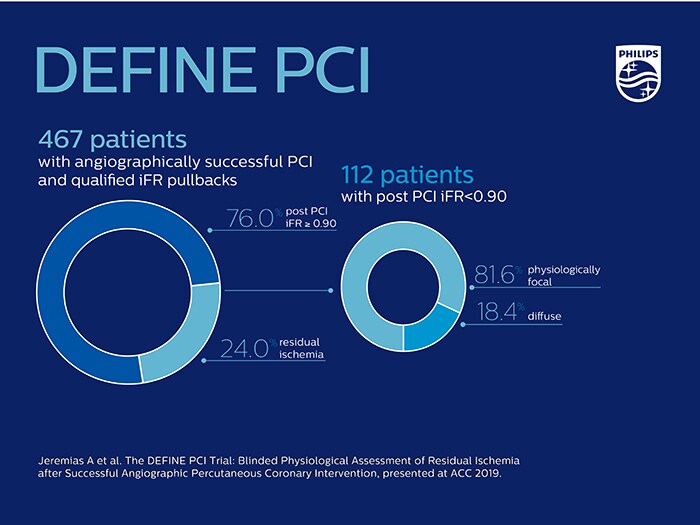
Amsterdam, the Netherlands and New Orleans, U.S. – At the American College of Cardiology’s (ACC) annual meeting in New Orleans, U.S., Royal Philips (NYSE: PHG, AEX: PHIA), a global leader in health technology, today announced the results of the DEFINE PCI [1] study, which assessed the level of residual ischemia found in patients after percutaneous coronary interventions (PCI). This study found that 1 in 4 patients [1] treated with standard of care PCI left the cath lab with residual ischemia (iFR < 0.90), as demonstrated by using a blinded iFR pullback measurement, which is Philips’ new physiologic guidance technology. Sponsored by Philips, the DEFINE PCI study involved approximately 500 patients, and was led by investigators from the Cardiovascular Research Foundation (US), Duke Clinical Research Institute (US) and the Imperial College London (UK). PCI is an image-guided, minimally invasive treatment to open a coronary artery blockage (stenosis) that is causing a reduced blood flow (ischemia) to heart tissue. Under interventional X-ray guidance (coronary angiography), clinicians navigate a balloon catheter and coronary stent to the treatment area to deploy them and restore the arterial blood flow. Several studies [2, 3] have revealed that a significant portion of patients treated with coronary stents continue to experience chest pain (angina) following PCI, leading to an increased rate of repeat procedures and corresponding higher costs. The DEFINE PCI study, which took place at centers throughout the US and Europe, shows that the current approach to PCI has limitations for identifying the locations of physiologically significant arterial lesions in patients suffering from coronary artery disease (CAD). Of the patients with residual ischemia, the study showed that 81.6% of those patients had an untreated focal stenosis (narrowing of an artery). Further analysis of the study data showed that if all focal stenoses had been identified and successfully treated, only 1 in 20 patients would still have residual ischemia. This indicates that if the precise locations causing ischemia are better detected prior to stenting, patient outcomes may be improved.
The findings from the DEFINE PCI study reveal an opportunity for physicians to optimize procedural results and potentially help more people fully benefit from PCI.
Allen Jeremias
MD, principal investigator of the DEFINE PCI study
“The findings from the DEFINE PCI study reveal an opportunity for physicians to optimize procedural results and potentially help more people fully benefit from PCI,” said Allen Jeremias, MD, principal investigator of the DEFINE PCI study. “The fact that nearly one-quarter of patients had residual ischemia despite an angiographically successful result, mostly due to focal lesions that can easily be treated, has important implications for improving outcomes of patients undergoing stent implantation globally,” said Gregg W. Stone, MD, Professor of Medicine at Columbia University Medical Center.
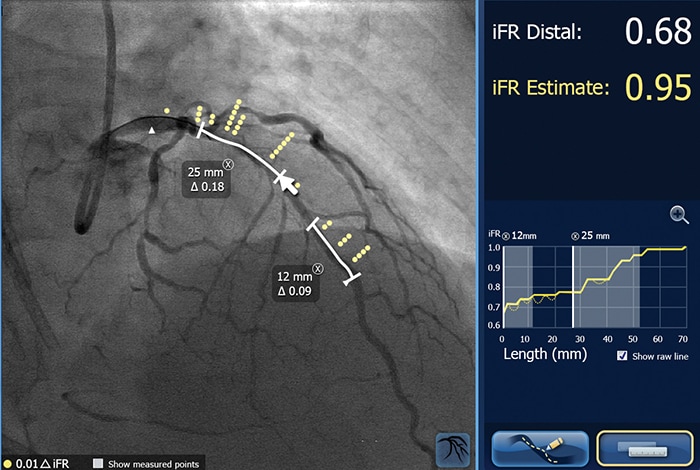
Tailored for advanced physiologic guidance
iFR is well established for determining whether a vessel is indicated for treatment through the landmark DEFINE FLAIR and iFR Swedeheart outcome studies, both published in the New England Journal of Medicine [4, 5]. The one-year patient outcomes were consistent with fractional flow reserve (FFR), while iFR involved less procedural time, reduced patient discomfort, and reduced cost [6]. Philips SyncVision iFR Co-registration further advances physiology by mapping the pressure profile of the whole vessel onto the angiogram, providing physiologic guidance for where to treat within the vessel. With iFR Co-registration, physicians can identify the precise locations causing ischemia, plan stent length and placement with a virtual stent, and predict physiologic improvement. Philips SyncVision with iFR Co-registration provides physicians with a full physiologic image allowing them to see clearly and treat optimally. “As iFR continues to be adopted into clinical practice, the DEFINE PCI study is the latest addition to mounting evidence that this innovative technology contributes to reducing costs, improving outcomes [4, 5, 7] and enhancing the patient experience,” said Christopher Barys, Business Leader Image Guided Therapy Devices, Philips. “With SyncVision with iFR Co-registration, we are providing physicians with the complete picture, allowing for more optimal treatment of their patients.” Philips SyncVision with iFR Co-registration is part of Philips’ unique portfolio of systems, smart devices, software and services in image-guided therapy, which combine to provide healthcare providers with sophisticated, procedure-oriented solutions. It is currently being showcased at ACC in booth #1901. Follow the #ACC19 conversation on @PhilipsLiveFrom throughout the event. More information about iFR Co-registration is available here. DEFINE PCI is the latest in a series of research on iFR techniques, building from the DEFINE FLAIR study in 2017, with economic results in 2018. [1] Jeremias A et al. The DEFINE PCI Trial: Blinded Physiological Assessment of Residual Ischemia after Successful Angiographic Percutaneous Coronary Intervention, presented at ACC 2019. [2] Recurrent angina after coronary angioplasty: mechanisms, diagnostic and therapeutic options. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3760523/ [3] Hakeem, A. Role of Postintervention Fractional Flow Reserve to Improve Procedural and Clinical Outcomes. Circ 2019; 139: 694-706. [4] Davies JE, et al. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N Engl J Med. 2017 May 11;376(19):1824-1834. [5] Gotberg M, et al. iFR Swedeheart Investigators. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. N Engl J Med. 2017 May 11;376(19):1813-1823. [6] Patel M. “Cost-effectiveness of Instantaneous Wave-free Ratio (iFR) compared with Fractional Flow Reserve (FFR) to guide coronary revascularization decision making.” Late-breaking Clinical Trial presentation at ACC on March 10, 2018. [7] Tonino, et al. Fractional Flow Reserve Versus Angiography for Guiding Percutaneous Coronary Intervention. N Engl J Med. 2009;360(3):213-224.
About Royal Philips
Royal Philips (NYSE: PHG, AEX: PHIA) is a leading health technology company focused on improving people's health and enabling better outcomes across the health continuum from healthy living and prevention, to diagnosis, treatment and home care. Philips leverages advanced technology and deep clinical and consumer insights to deliver integrated solutions. Headquartered in the Netherlands, the company is a leader in diagnostic imaging, image-guided therapy, patient monitoring and health informatics, as well as in consumer health and home care. Philips generated 2018 sales of EUR 18.1 billion and employs approximately 77,000 employees with sales and services in more than 100 countries. News about Philips can be found at www.philips.com/newscenter.
Topics
Contacts

Mark Groves
Philips Global Press Office Tel.: +31 631 639 916
You are about to visit a Philips global content page
Continue
Fabienne van der Feer
Philips Image Guided Therapy Tel: + 31 622 698 001
You are about to visit a Philips global content page
ContinueMedia assets
Press releases
Get our press releases by e-mail
You are about to visit a Philips global content page
Continue