Fifteen years ago healthcare innovation became my field of work – first as a research program manager, more recently as Chief Technology Officer. A lot has changed in this time span. Philips has evolved from a diversified electronics conglomerate into a focused health technology company – focusing on precision diagnosis, image-guided therapy, connected care and personal health. But what’s more, the way we innovate today is very different from how we used to. Healthcare systems around the world are grappling with a rising demand for care, staff shortages and unsustainable costs. If we are to make healthcare more affordable, accessible and effective, old methods of innovation simply won’t suffice anymore. As I reflect back on the past 15 years, I see five ways in which healthcare innovation has evolved.
1. Technology for healthcare innovation used to focus on product features – now it is about creating solutions for value-based care
When I entered this field, innovation in medical technology was mainly about improving the features of systems and devices. For example, I vividly remember the ‘CT slice war’, when Philips and other manufacturers competed on quality of CT scans by increasing the number of cross-sectional images (or ‘slices’) of a particular part of the body. From 16, to 32, then 64 and upward. The goal was straightforward: improve image resolution. The radiologist would benefit by being better able to identify abnormalities in a patient’s body. The dynamics of healthcare innovation would soon get more complicated. In 2005, the North American Deficit Reduction Act sent a shock wave through the world of medical imaging. Many imaging procedures were hit by reimbursement cuts. In hindsight, this was a first sign of things to come: the economics of care would become much more important. Simply improving the resolution of a CT scan was not enough anymore. Today, we see a shift to value-based care – which is about delivering on the quadruple aim of achieving better health outcomes, improved patient experience, improved staff experience, and lower cost of care. Product features are still important, but only as part of a broader solution. Fifteen years ago, we would go into a radiology department to showcase the performance and features of our latest scanner. These days a head of radiology may ask: how can you help my department become more efficient to meet growing patient demand? To answer questions such as this, innovation in healthcare needs to focus on integrated offerings of devices, software and services; moving from a product-centric to a solution-centric approach. For example, improving the efficiency of a radiology department may involve an analysis of equipment utilization and time it takes to read an image, benchmarking with other hospitals – using data to inform everyday decisions to boost quality and productivity. Measurable customer impact is now the yardstick for the success of an innovation. Or as our mantra has become: “It’s only a solution if it delivers on the customer’s KPIs.”

2. Aligned incentives have become critical in the transition to value-based care
Take hospital readmission management as an example. After being discharged from a high-risk incident, such as heart failure or pneumonia, patients have the highest risk of relapse during the first 30 days. According to the Agency for Healthcare Research and Quality (AHRQ), over $41 billion is spent each year on patient readmission within those 30 days. Telehealth technologies provide a way of connecting patients with caregivers beyond the walls of the hospital, via a combination of remote monitoring, ongoing education and self-management. This can help to lower costs while improving patient outcomes. However, legacy reimbursement models may still be tied to the number of patients visiting the hospital or the number of procedures performed – creating a perverse incentive to stick to the status quo. Thankfully, with the rise of value-based care, we see a shift in incentives from pay-for-procedure to pay-for-outcome. For example, accountable care organizations in the US may incur a penalty if a discharged patient is readmitted within 30 days – creating an incentive to extend care from the hospital to the home. First pilots with telehealth and hospital readmission management have shown promising results – with up to a 49.5% reduction in hospitalizations and 34.5% reduced cost of care [1]. To succeed with healthcare innovation today, new technologies must go hand in hand with new business models and outcome-based incentives that are aligned across all stakeholders – offering opportunities for long-term collaboration based on shared objectives and risks.
In the adoption of new technological innovations for value-based care, misaligned incentives have historically been the biggest barrier.
To succeed with healthcare innovation today, new technologies must go hand in hand with new business models and outcome-based incentives that are aligned across all stakeholders.
3. Solutions creation requires ecosystem innovation on open digital platforms
Over the past 15 years, the healthcare IT landscape has grown ever more complex. With an ongoing proliferation of systems and devices, there has never been a stronger need for all these disparate components to work together in a safe and cohesive way. This means technology vendors need to have an eye for the bigger picture. We can no longer assume that a hospital or health system will source all components of a solution from one vendor only. A company like Philips needs to be open to integrating with third-party offerings. We also need to be able to configure our solutions to the needs and context of a specific customer, with optimal reuse of standardized building blocks. This requires a common digital platform approach. Such an approach makes innovation more efficient, because it avoids duplication of building blocks across business silos. It also makes innovation more effective, by enabling interoperability and integration of solutions with existing hospital information systems and third-party offerings. The next step is to create a wider ecosystem of innovation, by opening up our platforms to third parties (in a safe and well-controlled way, of course). With the rise of AI, there’s a plethora of apps coming from start-ups and universities. But hospitals may find it hard to put these apps to use if they lack a common underlying platform that is integrated with their workflow at the point of care. As one CIO of a large hospital network said during our recent AI Startup Program: “I run about 10,000 applications at 150,000 different terminals. The one thing I do not want is more applications I need to manage.” This is where companies such as Philips can step in. Increasingly, hospitals want us to act as an integrator and broker of technology. With the to-be-launched Philips Marketplace, this is precisely what we aim to offer – helping healthcare providers to embed third-party apps into their workflow via a common underlying deployment platform.

Startups discussing AI solutions for healthcare during our AI Startup Program
4. Patient data used to reside in systems of record – now we need a system of engagement, bringing a 360-degree view of the patient into clinical workflows
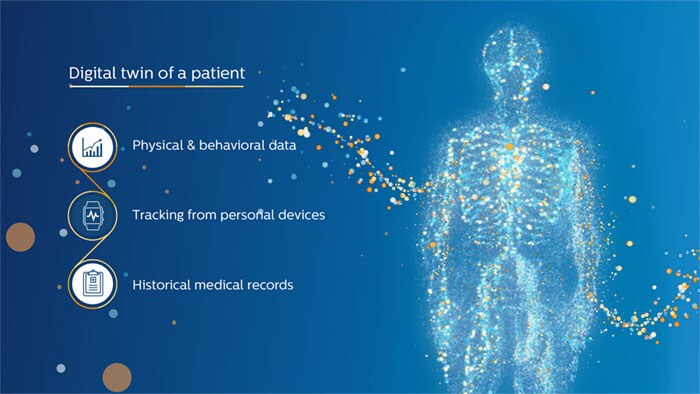
Traditionally, healthcare data resides in disparate silos. The data is typically not annotated or curated. It doesn’t capture the full clinical context either. Over the past 15 years, the more widespread introduction of the Electronic Medical Record (EMR) has created a system of record to keep track of clinical decisions and to support billing. But the EMR has not made patient data flow between caregivers; nor does it guide them with actionable insights. What we need instead is a system of engagement, which connects and interprets patient data from various sources to support caregivers with relevant insights at the point of care. The development of patient monitoring in the general ward serves as a case in point. Historically, each of a patient’s vital signs – such as heart rate and blood pressure – was tracked manually. Today, these data can be automatically integrated and interpreted with smart algorithms to identify when a patient is at risk of deterioration – helping nurses to act swiftly when needed. One study showed that this can lead to a reduction in cardiac arrests of more than 86% [2]. As we continue to connect data across devices, departments and episodes of care, the ultimate vision is to have a digital twin of a patient: a model that integrates all relevant information about the patient, and that is updated over time. Digital twins have already shown promise in diagnosis and treatment of heart conditions. Ultimately, they have the potential to offer a 360-degree view of the patient at the point of care. Healthcare will become more precise and personalized as a result.
As systems and devices in healthcare are getting more integrated, the importance of connecting data across the continuum of care has also moved to the forefront.
5. Research has moved to the frontline of innovation – working closely with customers and across businesses
Because the nature of health technology innovation has changed, our research organization also looks very different from 15 years ago. Innovation used to be a sequential process, with central research labs working in relative isolation on concepts for new or improved devices or systems, following a technology roadmap. We would then transfer these concepts to product divisions in Philips, who would develop them further and push them to the market in a one-size-fits-all manner. Nowadays, innovation is a more parallel process, which occurs in collaboration with customers. For example, we are working side by side with researchers from Karolinska University Hospital in Sweden on innovations in minimally invasive surgery, prostate cancer care and stroke care. We have similar research partnerships around the globe. This collaborative approach calls for a different mindset. As a researcher, you cannot focus on technology alone anymore. You also need to have an understanding of value propositions, health economics, market dynamics, and local digital ecosystems. As we like to say within Philips: "not the lab is your world, the world is your lab". That is why we set up four regional innovation hubs – in Cambridge (US), Shanghai (China), Bangalore (India) and Eindhoven (The Netherlands). This model promotes cross-functional collaboration on a regional level – bringing together knowledge on technology, digital platforms, clinical workflows, IT, finance and market access.
Not the lab is your world, the world is your lab.

In discussion with Philips researchers during a recent visit to our Shanghai innovation hub
In addition, we now work with a much broader group of stakeholders in hospitals and health systems: not only technical specialists, but also heads of department and board members. This means you have to be able to speak the languages of different stakeholders – a much more versatile and challenging role! To ensure that customers get the integrated solutions they are looking for, our research organization has also taken a much more proactive role in connecting different business units within Philips. For example, in oncology, we are bringing together the latest advances in imaging, digital pathology, genomics and clinical informatics, to support precision diagnosis and therapy planning. This requires many different experts to work together. You can’t just innovate per business unit anymore – integration is now the name of the game.
The road ahead
Looking back on the changes of the last 15 years, I am once again struck by the tremendous progress that medical science and technology have made – resulting in amazing capabilities for diagnosis and treatment, and a positive impact on society. But it has also become clear that to achieve the quadruple aim, we now need a new approach to innovation. It will be the only way to keep high-quality healthcare sustainable for those who already have access to it, and to eventually make it available to all – for generations to come. References [1] Dahl, D., Khurana MD, H. (2015). Impact of an intensive ambulatory program on both financial and clinical outcomes in Banner Health, revisit the initial cohort with extended follow-up. Unpublished internal study. [2] Subbe, C.P., Duller, B. & Bellomo, R. Crit Care (2017) 21: 52. doi:10.1186/s13054-017-1635-z
Share on social media
Topics
Author

Henk van Houten
Former Chief Technology Officer at Royal Philips from 2016 to 2022













