In October 2019, Philips’ Chief Innovation & Strategy Officer Jeroen Tas presented his vision of the ‘Hospital of the Future’ at the HLTH Conference in Las Vegas. It’s a vision of a hospital not confined behind the walls of a single building or hospital complex, but a hospital comprising an integrated network of healthcare facilities and services reaching out into every corner of the community. One where integrated data flows seamlessly, and care is always on 24/7. Where artificial intelligence (AI) helps doctors to understand the complexity of the drivers that underlie our individual health, and where adaptive human-centered technology supports each of us along the journey to health and wellness. In the blog post below, Jeroen Tas, Chief Innovation & Strategy Officer at Philips, shares his views on this exciting shift in the way healthcare is delivered.
Unique individuals, unique healthcare needs
Each and every one of us is unique. That equally applies to our health, and it’s not just down to our genes or the epigenetics that turn those genes on and off. It is also related to factors such as living in safe housing, benefiting from a steady income, receiving a good education, having access to quality healthcare and adopting healthy lifestyle behaviors, such as eating nutritious food, enjoying good sleep, lowering our stress levels and alcohol-intake. These are what the World Health Organization describes as ‘the social determinants of health’. For chronic diseases, such as diabetes, COPD and congestive heart failure, these factors play a large part in determining the disease’s onset, progression and outcome. If our health is influenced by so many different factors, it follows that optimizing outcomes requires a holistic approach that centers on us as unique individuals. Discharging a patient back home is of little use to them if their home is ill-equipped to cope with their daily needs, or if access to adequate homecare is lacking. Yet today’s hospital systems aren’t always centered around people. More often, they are centered around episodic acute care, medical specialisms and technologies – much focus on medical expertise, not enough on people’s health journeys and experiences.
What if hospitals could use connected devices and streaming data to monitor patients 24/7 from a virtual care center? What if we could combine personal medical data with socio-economic and behavioral data to predict health risk and potential deterioration? What if family, friends and the community could participate in care? The combined benefits to individuals, their families and to society at large would be enormous.
Jeroen Tas
Chief Innovation & Strategy Officer, Philips
Fortunately, things are beginning to change. Many of the world’s leading care providers have started to organize themselves around their patients’ clinical and social needs, joining the dots between the different disciplines involved in an individual patient’s health journey and combining all the data points – medical, social and environmental – that characterize where the patient has come from, where they are now, and where they are likely to go. What if hospitals could use connected devices and streaming data to monitor patients 24/7 from a virtual care center? What if we could combine personal medical data with socio-economic and behavioral data to predict health risk and potential deterioration? What if family, friends and the community could participate in care? The combined benefits to individuals, their families and to society at large would be enormous.

In addition to providing more personalized and predictive care, there are other good reasons why the current hospital-centric model of care delivery will gradually change. Virtually every country in the developed and developing world is facing rising demand for care from growing and aging populations, coupled with escalating healthcare costs and staff shortages. On its current trajectory, the world will simply not have enough human and financial resources to deliver quality care via the traditional bricks-and-mortar hospital or nursing home model. Several studies have suggested [1] that better care at home for those that represent the largest cost to the system – elderly people with multiple chronic diseases – has a positive impact on patient wellness and stability, while dramatically reducing emergency care and hospital readmissions.
The rise of Integrated Delivery Networks
The drive for efficiency is already leading to consolidation and the growth of Integrated Delivery Networks (IDNs). These are stakeholder groups, such as hospitals, doctors’ offices, homecare providers and payers, that work collaboratively to ensure a more coordinated patient journey. At the same time, a new generation of tech-savvy patients has emerged, who are more than capable of tracking and piloting their own health and wellness. This new breed of healthcare consumer will expect the same convenience in their healthcare experiences that they already get in other aspects of their life, such as their banking or on-line purchasing. In control of their own health data, they will expect to share decision making with healthcare professionals rather than simply ‘doing what the doctor says’. To address these expectations, we already see retailers such as WalMart, CVS, Walgreens, BestBuy and tech companies like Apple, Amazon, Google and Microsoft getting into healthcare. However, improving population health outcomes and reducing costs is not enough. The so-called ‘quadruple aim of healthcare’ also calls for improvement of both the patient and the care professional experience. Studies show that patients who have a better experience of care generally have better health outcomes, and healthcare providers that offer a better staff experience benefit from higher quality, lower burn-out rates and lower staff turnover ratios. Philips’ Ambient Experience solutions for radiology departments and its family-friendly Neonatal Intensive Care Unit (NICU) solutions are good examples of how all four elements of the quadruple aim can come together in an integrated solution.
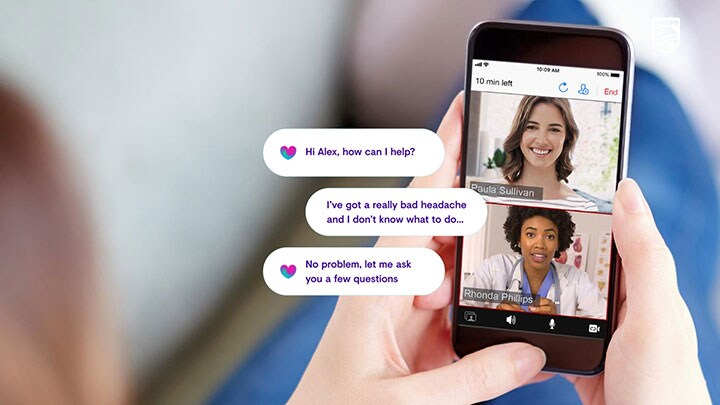
The hospital of the future will no longer be one large building that provides costly in-patient care for a broad range of diseases. Over the next five to ten years, what we conventionally think of as hospitals will increasingly be reserved for the most acutely ill patients and for highly complex procedures. Preventative care and routine treatment for the rest of the patient population will be delivered via connected hubs and spokes in a healthcare network that includes local retail clinics, same-day surgery centers and cath labs, specialist treatment hubs, freestanding emergency rooms, and even people’s homes – a networked ecosystem joined together by people, places, devices, software and services interwoven throughout communities. Clinical and Operations (Command) Centers will continuously analyze demand and supply, and the associated patient flows in the network, in real time. They will use AI to provide predictive insights that enable the removal of bottlenecks in care, and use it to identify patterns in the data that support better targeted population health management, helping to identify and protect vulnerable individuals before their health deteriorates. At the same time, virtual care (telehealth) solutions will leverage the network to monitor vulnerable patients 24/7 in their own homes.
Local expertise, global reach
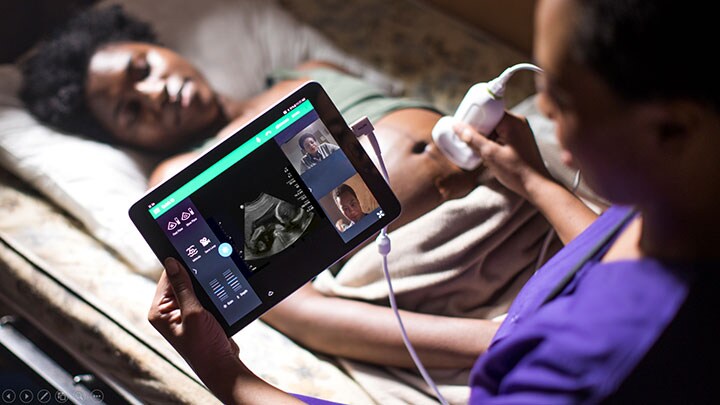
These networked solutions will not only serve the communities in which they are based. They also have the potential to span vast distances. In collaboration with the PURE (Point-of-care Ultrasound in Resource-limited Environments) initiative, Philips is already deploying a unique tele-ultrasound program that allows physicians based in Europe and the US to support emergency medicine physician training thousands of kilometers away in Rwanda, Africa, helping to boost the country’s emergency medicine capabilities. Via its ICU command center (eICU) solutions, Philips is helping Emory Healthcare day-time intensivists and critical care nurses based at Macquarie University’s MQ Health in Sydney, Australia, to deliver night-time care to ICU patients back in the US 15,000 km away. The program doesn’t replace night-shift staff in the US, but it alerts them to patients that are showing signs of deterioration and offers them expert guidance on the necessary interventions. With our IntelliSpace Precision Medicine solutions, hospitals around the world will have access to Dana Farber’s expert oncology pathways and specialists, bringing the best in cancer diagnosis and treatment guidance to community hospitals that do not have the expertise to keep up with today’s rapid progress in cancer care.
The important thing is that, however diverse or geographically distributed these networks are, what binds them together are the experiences of the people they serve. Seamless and personalized experiences for patients and healthcare professionals alike. It’s the hospital of the future that could guide us all towards better health.
Share on social media
Topics
Author

Jeroen Tas
Chief Innovation & Strategy Officer Jeroen is an experienced global executive and entrepreneur with a track record of leading innovation in the healthcare, information technology and financial services industries. Leading the company’s global Innovation & Strategy organization, he’s responsible for creating a pipeline of innovative business propositions that address emerging customer needs and enable a high-growth, profitable health continuum strategy.
Follow me on














