A year ago, I wrote about how technology is rapidly transforming stroke care, a welcome development in combating a disease that claims approximately 6 million lives around the world each year [1]. I promised to revisit this important topic to examine the latest advances in how the medical community is dealing with this life-altering disease. In this article, I take a closer look at the full cycle of care and how we could optimize workflows to help improve how we diagnose and treat stroke. Across the globe, smart solutions are put to work by world-class stroke centers, to support staff in delivering the best outcomes they can for their patients. My fellow physicians don’t need me to make the case for why improving health outcomes is always our primary goal.
Across the globe, smart solutions are being put to work by world-class stroke centers, to support staff in delivering the best outcomes they can for their patients.
Atul Gupta, MD
Chief Medical Officer, Philips, Image Guided Therapy
The quadruple aim in health care necessitates us to improve the patient experience while reducing cost of care. Health systems are increasingly working under value-based care models. This means they’re being measured not only on health outcomes, but also on what matters to the patient – things like their experience during diagnosis, treatment and quality of life.
Prevention first
With key treatable or modifiable risk factors for stroke including hypertension, tobacco use, physical inactivity and obesity, it’s not surprising that up to 80% of strokes could be prevented through lifestyle changes [2]. Another leading risk factor for stroke is atrial fibrillation (Afib), widely regarded as a global public health problem: 33.5 million people around the world are currently living with this condition that increases their risk of stroke five-fold [3, 4]. If we can treat Afib more effectively and efficiently, we can reduce the likelihood of stroke happening in the first place. Coupling our image-guided therapy expertise with our novel KODEX-EPD system has the future potential to address the key unmet need of real-time therapy assessment during Afib ablation procedures, lowering its recurrence and helping us get ablation ‘first time right.’
Reducing time to treatment
If a patient does have a stroke, every 30 minutes’ delay before treatment reduces the chance of a good outcome by 14% [5]. We know time is brain. Every minute of cerebral ischemia results in the death of 2 million neurons [6]. Each hour of delay ages the brain by 3.6 years compared to a normal-aging brain [7]. That’s why I think it’s so crucial to be able to diagnose patients and get them the intervention they need, as swiftly as possible.

Each hour of delay in treating stroke ages the brain by 3.6 years compared to normal-aging brain.
Atul Gupta, MD
Chief Medical Officer, Philips, Image Guided Therapy
We’re working to shorten the path to diagnosis and treatment in several ways – before the patient even gets to the Azurion interventional suite. We support hospitals in leveraging their resources to quickly deliver life-saving interventional procedures to those who need them most. We are working with leading stroke centers to develop innovations, aimed at improving the image quality further, and to improve workflow to shorten re-perfusion time after ischemic stroke [8] (you can learn more about this here).

Improved understanding, better outcomes
While tracking measurements like door-to-thrombectomy time is critical, I believe that looking at that metric alone may be shortsighted. The value for the patient is created across the full cycle of care – from their pre-hospital experience, throughout their time in the hospital, as they are teed-up for discharge, and during their recovery period at home. Our experience flow mapping technique helps to build a vivid picture of what’s going on, establish what’s working well and what’s not, and, ultimately deliver more targeted solutions. Rural communities and those with underequipped health facilities are typically most in need of improvement. Thankfully, new solutions in telemedicine are improving access to care, enhancing diagnosis, reducing costs and improving outcomes. Telestroke programs, where stroke experts work with the emergency team in rural areas over the phone or via video to help diagnose and recommend treatment, have been shown to cut ‘stroke-to-needle’ time in half [9]. Indeed, our telehealth partnership with Northwell Health saw ICU mortality reduced by up to 20% and double the number of patients assessed and prescribed the life-saving clot-busting drug tPA [10].
What’s next?
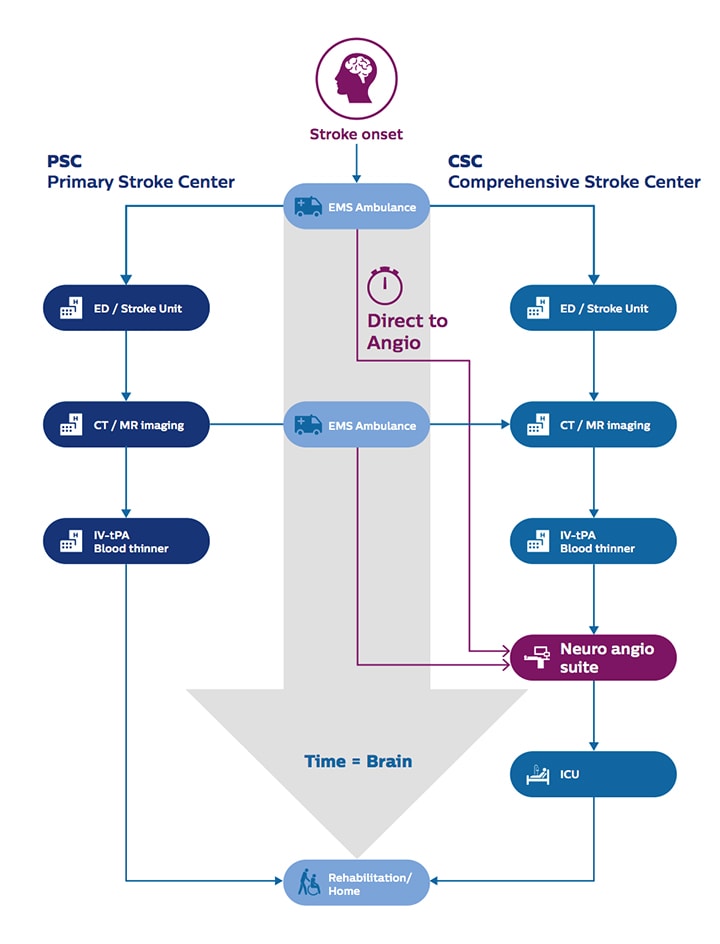
The DAWN and DEFUSE 3 trials have initiated new treatment pathways that are set to revolutionize how we can treat stroke patients. The widening indications for thrombectomy allow us to deliver mechanical thrombectomy to more patients than ever before, potentially reversing the devastating effects of stroke and significantly improving quality of life. On the other hand, these trials have resulted in a sharp increase in patient volumes as many more patients are now eligible candidates for stroke thrombectomy. Thus, we must improve efficiency in care delivery, while simultaneously decreasing time to thrombectomy. The upcoming WE-TRUST ‘Workflow optimization to rEduce Time to endovascular ReperfUsion in Stroke Treatment’ study will assess the impact of a Direct to Angio Suite (DTAS) workflow on stroke patient outcomes. Several studies [11, 12, 13] have already indicated that having this ‘one-stop-stroke shop’ DTAS workflow can sizably reduce time to treatment and improve outcomes.
As I mentioned a year ago, the fight against stroke remains one that must be waged on multiple fronts and I am more enthused than ever to see such rapid progress in this fast-moving field of stroke therapy.
References: [1] Global Health Estimates 2016: Deaths by Cause, Age, Sex, by Country and by Region, 2000-2016. Geneva, World Health Organization; 2018. Available at https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death. [2] Centers for Disease Control and Prevention. (2018). Preventing Stroke: Healthy Living. Available at https://bit.ly/2NCRZ4k [3] Atrial fibrillation and stroke: unrecognised and undertreated. The Lancet. (2016). Available at https://bit.ly/2X2dKgK [4] The Stroke Association. (2018). State of the Nation report. Available at https://bit.ly/2Q9armK. [5] https://www.ahajournals.org/doi/10.1161/STROKEAHA.118.021989 [6] Stroke. 2006; 37: 263-266. [7] https://www.ncbi.nlm.nih.gov/pubmed/16339467 [8] Borja I, Stefan J, Stefan A, et al., ESC Scientific Document Group, 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. European Heart Journal, Volume 39, Issue 2, 07 January 2018, Pages 119–177, https://doi.org/10.1093/eurheartj/ehx393 [9] Müller-Barna P, et al. TeleStroke Units Serving as a Model of Care in Rural Areas 10-Year Experience of the TeleMedical Project for Integrative Stroke Care. Stroke. 22014; 45(9): 2739-44. [10] Philips (2018). Northwell Health improves patient care and satisfaction with Philips integrated patient monitoring solutions. [11] Ribo M, Boned S, Rubiera M, et al. 2018 Mar;10(3):221-224. doi: 10.1136/neurintsurg-2017-013038. Epub 2017 Apr 26 [12] Jadhav AP, et al. Stroke. 2017;48:1884-1889
Share on social media
Topics
Author

Atul Gupta
Chief Medical Officer, Image Guided Therapy Atul Gupta, MD is Chief Medical Officer at Philips’ Image Guided Therapy and a practicing interventional radiologist. Prior to joining Philips in 2016, Atul served on Philips’ International Medical Advisory Board for more than 10 years. Atul continues to perform both interventional and diagnostic radiology in suburban Philadelphia, in both hospital and office-based lab settings. He has been repeatedly recognized as top physician for his specialty in the media and serves on several advisory boards. He has also published and lectured internationally on a range of interventional procedures.
Follow me on













