Seven key benefits of AI in healthcare for patients and healthcare professionals
Dec 16, 2025 | 3 minute read
Artificial intelligence (AI) is rapidly reshaping the healthcare industry, offering new ways to analyze patient data, support healthcare professionals and enhance patient care. While its full potential is still untapped, real-world use cases already show tangible impact. From accelerating diagnostic imaging to supporting clinical decision-making and enabling more preventive care, the benefits of AI in healthcare reach every aspect of care delivery. Here are seven ways AI can make a difference for patients and healthcare professionals alike.
1. Saving time by streamlining administrative tasks
Every day, healthcare professionals go above and beyond for their patients, yet many find their time and energy drained by an ever-growing burden of administrative work. The Philips Future Health Index 2025 report shows that more than one-third of healthcare professionals now spend less time with patients and more on paperwork compared to five years ago, while only 20% get to spend more time with patients. This shift is taking a heavy toll on their well-being: healthcare professionals who spend less time with patients than they did five years ago feel significantly more stressed compared with their peers.
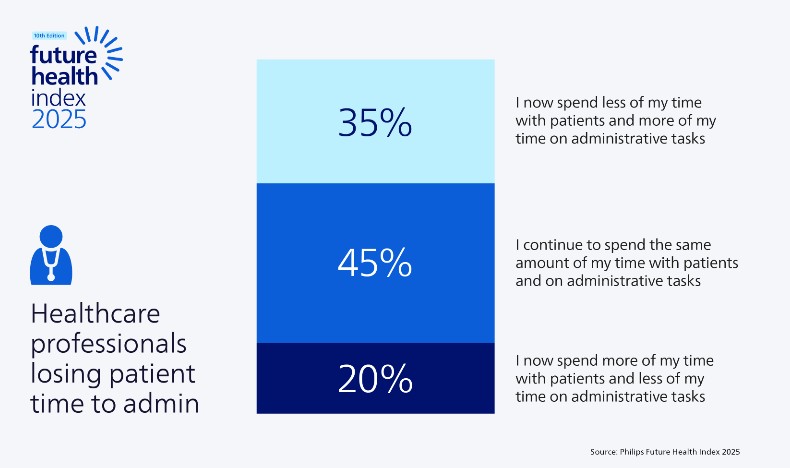
That’s where AI implementation in healthcare can make one of its most immediate contributions: by automating time-consuming administrative tasks and freeing up time for patient care. In fact, healthcare professionals in the Future Health Index 2025 report say it’s where they expect the biggest positive impact from AI in their department, along with improving access to clinical research.
In recent years, a range of innovations has emerged to streamline administrative workflows in healthcare. Generative AI tools, for example, can now transcribe interviews, summarize patient notes, and automatically draft reports or referral letters. By minimizing manual data entry and documentation, these technologies can enable healthcare professionals to devote more time to patient care and less time to administrative tasks.
2. Speeding up diagnostic exams and image processing
Radiology departments face increasing pressure to handle growing patient volumes while maintaining high-quality medical images. That’s why many are implementing AI to improve operational efficiency, improve image quality and ease the workload of radiologists and staff. For example, computed tomography (CT), which is one of the most widely used medical imaging modalities, can benefit significantly from AI-powered tools that streamline workflows and enhance image quality, helping departments do more with the resources they have. A similar transformation is underway in magnetic resonance (MR) imaging. As demand for MR scans rises, AI-based image reconstruction can help healthcare providers scan more patients in less time and produce sharper, high-resolution images. By accelerating exam times and enabling first-time-right scans across a wide range of patient conditions, AI also enhances the patient experience – especially for those who are anxious or in pain – making advanced medical imaging more accessible and less stressful.
AI can enhance every stage of the CT imaging workflow, starting with patient positioning – a critical step where inaccuracies can result in higher radiation doses or image noise. AI-enabled camera technology can automatically identify anatomical landmarks to support accurate and consistent alignment. Combined with AI-driven image reconstruction, these technologies can help reduce radiation exposure while producing clearer images that strengthen diagnostic confidence.
3. Elevating the skills of less experienced staff
Another key benefit of AI in healthcare highlighted in the Future Health Index 2025 report is its ability to help less experienced staff perform diagnostic exams with greater accuracy and consistency. This kind of AI-enabled support is especially valuable at a time when qualified healthcare professionals are in increasingly short supply, particularly in underserved regions and communities. In cardiac care, for example, ultrasound has become an indispensable tool for visualizing and evaluating heart function. Yet, the quality of ultrasound imaging often depends heavily on the operator’s experience. Certain measurements required in every echocardiography exam can be time-consuming and subject to considerable inter- and intra-operator variability. AI can help address these challenges by reducing manual and repetitive tasks, much like in other areas of healthcare. AI-based automatic measurements can enable fast, reproducible, and consistent quantification of cardiac function, improving both the patient and staff experience. Clinicians can review, accept, or adjust these measurements based on their own assessments, giving them a powerful tool to enhance their human expertise while maintaining full control over diagnostic decision-making. In practice, AI-enabled ultrasound systems can even provide real-time image quality feedback during cardiac scans. This supports higher diagnostic confidence and broadens access to quality care by empowering more users, across a wider range of care settings, to help them perform successful ultrasound exams.
4. Enhanced diagnostic accuracy and early detection
Beyond automating and accelerating routine tasks, AI is increasingly becoming a powerful clinical decision-making support tool – analyzing medical images, identifying subtle patterns and surfacing insights that might otherwise go unnoticed. By augmenting the expertise of radiologists and other medical professionals, AI can turn vast amounts of patient data into actionable information, helping clinicians to make faster and more confident decisions that can ultimately help improve patient outcomes. For example, AI-powered image analysis can contribute to the early detection of clinically relevant breast cancer and help reduce screen-reading workload [1]. Similarly, AI-based lung nodule detection can perform nodule search 26% faster, detecting 29% of previously missed nodules compared to manual inspection [2]. Such advances are especially valuable for conditions where early detection is closely linked to improved health outcomes. At the same time, appropriate human oversight remains essential to ensure that AI is applied safely and responsibly in medical imaging analysis. Our Future Health Index 2025 report shows that patients are less comfortable with the use of AI in diagnostic decision-making than with its use for administrative tasks, such as scheduling or check-in. This underscores the vital role of healthcare professionals in helping patients understand how AI supports, rather than replaces, clinicians’ expertise in medical diagnosis and healthcare delivery.

5. Supporting more personalized treatment plans
AI systems are opening new possibilities for personalized patient care by drawing insights from vast and varied sources of health data. By analyzing information from electronic health records, imaging studies and even patient-generated data, AI algorithms can help clinicians gain a more holistic view of each patient’s medical history and current condition. This deeper understanding can support more precise, individualized decision-making at every stage of care. One area of rapid progress is the use of natural language processing (NLP), which enables AI systems to extract clinically relevant insights from unstructured data, such as physician notes or discharge summaries. When combined with structured data from electronic health records, these insights can reveal subtle patterns or risk factors that may not be immediately apparent. This allows healthcare teams to identify the most effective diagnostic or therapeutic options tailored to each patient’s unique needs [3]. Importantly, these AI tools are not intended to replace clinical expertise but to complement existing clinical guidelines. By combining data-driven insights with the human expertise of healthcare professionals, AI can help enhance treatment precision and ultimately contribute to better patient outcomes.
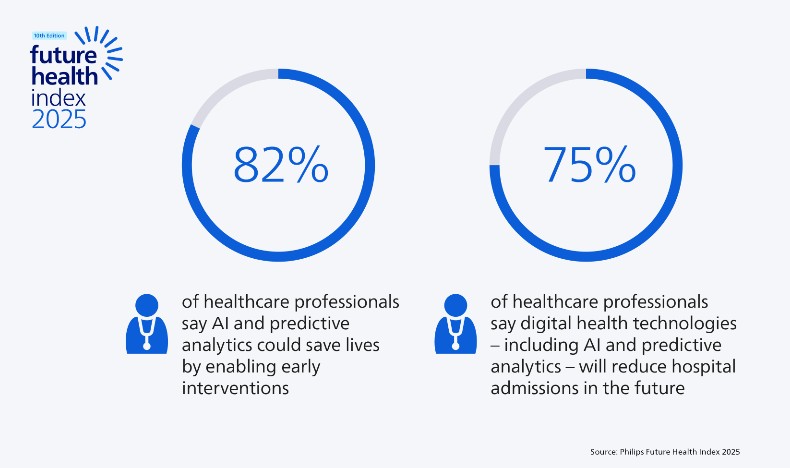
6. Enabling more predictive and preventive care
Among the most promising benefits of AI in healthcare is its ability to help prevent the need for certain types of patient care altogether. As chronic disease rates rise and healthcare costs continue to escalate, governments and healthcare organizations are shifting their focus from reactive to proactive care models. By implementing AI tools in healthcare, providers can move toward early detection and prevention, helping to improve patient outcomes while making more efficient use of healthcare services and resources. The Future Health Index 2025 report highlights this transformation: 82% of healthcare professionals believe that AI and predictive analytics could save lives by enabling early interventions, and 75% say these technologies will help reduce hospital admissions in the future. AI models can identify subtle trends and risk factors in large volumes of health data, alerting clinicians to potential complications before they become acute. By anticipating patient needs earlier, healthcare organizations can deliver more timely, targeted interventions that can help reduce costs and enhance the overall quality of care.
This shift is already taking shape in areas such as cardiac care. As healthcare increasingly extends beyond hospital walls into homes and communities, AI can analyze data collected remotely through medical-grade wearables and other connected devices. For example, cloud-based AI can help interpret electrocardiogram (ECG) readings to detect atrial fibrillation or other heart rhythm disturbances that might otherwise go unnoticed. By flagging irregularities that require urgent attention, clinicians can act sooner, which can help prevent deterioration and improve outcomes.
7. Supporting personalized self-care
AI technology is not only transforming clinical workflows but also empowering individuals to take a more active role in their own health and well-being. Through continuous, data-driven insights, AI can enable proactive health monitoring and help people better understand how lifestyle factors such as sleep, diet, and physical activity influence their overall condition. As healthcare becomes increasingly connected, these tools can complement professional care with more personalized self-care, supporting better prevention, early detection and management of chronic diseases. Virtual health assistants are an example of this shift [4]. By combining conversational interfaces with advanced AI models, they can provide personalized reminders, guidance and mental health support, helping patients stay engaged in their treatment plans. When integrated into broader care pathways, they could offer a bridge between self-management and professional oversight, potentially improving both patient engagement and health outcomes. At the same time, integrating AI into personal health monitoring raises important questions around data security, privacy and psychological well-being. Over-monitoring could lead to unnecessary anxiety, and safeguarding sensitive patient information remains paramount [5]. To build trust, grow AI adoption and ensure responsible use, we must apply robust ethical principles that protect privacy while preserving the benefits of AI-enabled technologies for patients and healthcare professionals alike.
Sources [1] https://www.thelancet.com/journals/landig/article/PIIS2589-7500%2824%2900267-X/fulltext [2] https://www.usa.philips.com/healthcare/product/NICA555/ct-lung-nodule-analysisclearreadcad [3] https://pmc.ncbi.nlm.nih.gov/articles/PMC11475376/
Share this page with your network








