AI in radiology: three keys to real-world impact
Nov 20, 2025 | 4 minute read
Radiology has been at the forefront of AI innovation ever since the earliest medical imaging analysis models began showing clinical promise. From breast cancer detection to lung nodule identification, the field has served as a proving ground for what AI tools can do in healthcare. Yet turning its full potential into practice remains a challenge. Too many AI technologies stall at the pilot stage or struggle to earn radiologists’ trust. The question is no longer whether AI can add value, but how to make it work in radiology practice to effectively support radiologists – and, ultimately, help deliver better patient care.

A growing need for efficiency in medical imaging
“We don’t just need more pixels; we need more productivity.” That insight from a radiology leader captures a growing and pressing reality in medical imaging. While radiology departments continue to benefit from incremental improvements in image quality and resolution, their most urgent need is for AI solutions that improve efficiency, enhance capacity, and ease the pressure on overstretched radiologists – all while maintaining diagnostic accuracy. Time has become the scarcest resource in diagnostic imaging. Patient volumes are rising faster than staffing levels, creating a gap that will only continue to grow as populations age. More than one-third of radiologists report symptoms of burnout [1], while 77% of healthcare leaders said care delays due to staff shortages are affecting patient outcomes [2]. Across health systems, backlogs in diagnostic studies are taking a toll – delaying diagnosis and treatment decisions and increasing anxiety for patients seeking clarity and reassurance. The situation is compounded by the complex nature of modern medical imaging. The number of images per study has increased exponentially over the past decade. A single CT exam, for example, can now contain thousands of slices. Radiologists must interpret more data than ever, facing a deluge of patient information but a dearth of actionable insights. At the same time, the pace of medical research is accelerating so rapidly that staying current with new evidence, imaging protocols, and diagnostic criteria has become a challenge in itself, adding yet another layer of complexity to an already demanding role.
Radiologists optimistic about AI, but barriers to adoption remain
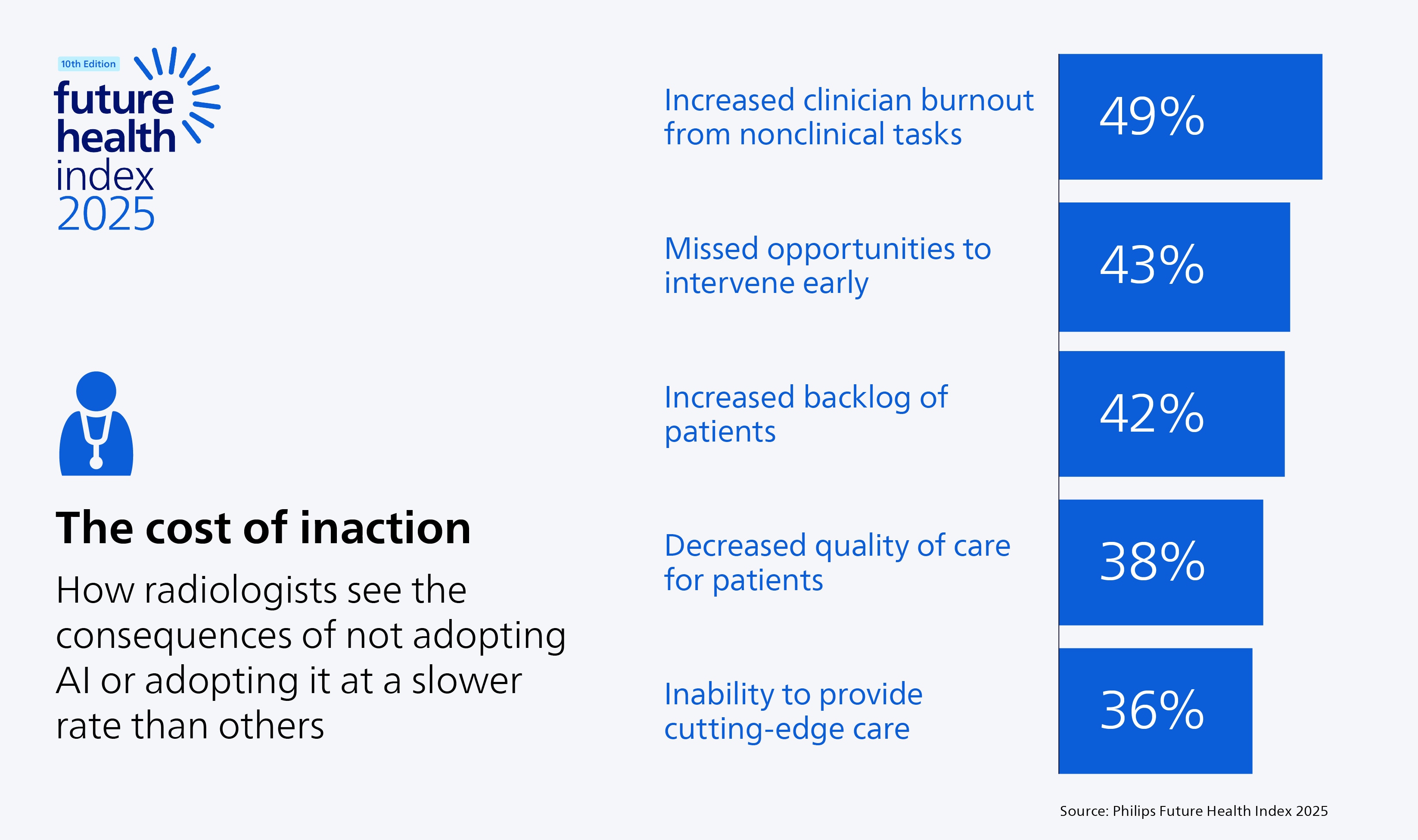
With today’s shortage of qualified professionals, hiring more radiologists and staff typically isn’t an option. That’s why healthcare providers are turning to AI to help their existing teams do more with the resources they have. When thoughtfully designed and implemented, AI systems promise to make radiologists’ work both more efficient and more consistent. The Philips 2025 Future Health Index reflects this optimism: 85% of radiologists believe AI will help ensure greater consistency in patient examinations, with the same number saying it can ultimately improve patient outcomes. Radiologists are also clear about the cost of inaction. They say that those not adopting AI – or doing so more slowly than others – risk worsening clinician burnout from administrative overload, missing opportunities for early intervention, and allowing patient backlogs to grow.
But optimism alone is not enough. Despite widespread belief in AI’s potential, real-world adoption still lags expectations. Studies show that many AI tools in radiology remain confined to pilot projects or narrow use cases that don’t scale well, often due to poor workflow integration, lack of trust or limited interoperability in clinical practice, among other reasons [3]. Real-world case studies show that delivering tangible impact on patient care with AI depends on getting three things right: designing radiology AI around human needs, embedding it deeply into everyday workflows, and building trust among radiologists, referring physicians, and patients. We’ll explore each in more detail.
1. People first: designing AI tools that solve real problems
For AI in radiology to make a real impact, it must start with the people who use it. The 2025 Future Health Index shows that while 78% of radiologists have been involved in developing new technologies at their organization, 41% feel those tools don’t adequately address their real-world needs. Too often, AI innovation begins with building machine learning algorithms or deep learning models before fully understanding the human workflows they are meant to support. As a result, adoption in radiology practice often lags despite impressive AI performance in controlled research settings [4].

The most effective AI tools put people first. They automate repetitive and administrative tasks, freeing radiologists to focus on image interpretation, patient communication and multidisciplinary collaboration. Not as a replacement for human expertise, but as an enhancer of it. When designed around the needs of radiologists, AI can streamline routine work and augment human capabilities across the entire radiology workflow. Let’s examine several real-world examples.
Reducing administrative burden with AI solutions
Radiologists today spend an increasing share of their time managing patient data, reports, and scheduling. These are all tasks that could at least be partly automated. In the 2025 Future Health Index, 43% of radiologists said they now spend less time with patients and more on administrative work than five years ago, compared to only 14% who say they now get to spend more time with patients. Generative AI is beginning to help ease that burden. For example, by assisting in turning spoken dictation into structured reports, with the appropriate human oversight, AI can help reduce the documentation load and free up time for radiologists to focus on patient care.
Accelerating image acquisition and reconstruction
AI-enabled systems are also transforming the acquisition of medical images. For example, at KMC Manipal Hospital in India, AI-enabled CT workflows have empowered clinicians to serve 20 to 30 more patients daily while maintaining diagnostic accuracy and image quality of CT scans. Similarly, AI-enabled MR processing uses deep learning reconstruction to improve both speed and quality, reducing scan times and motion artifacts even in complex areas like cardiac or pediatric imaging. By accelerating image acquisition, technologists can potentially perform more studies per day, while radiologists can gain access to higher-quality data sooner. This translates into both a more efficient radiology department and a better experience for patients.

Streamlining interpretation through AI-enabled image segmentation
Accurate image segmentation is essential in diagnostic imaging, from outlining tumors to quantifying organ volumes or assessing cardiac structures. Traditionally, this process has been manual and time-consuming, adding to radiologists’ workload. AI-based segmentation tools can now automate much of this effort. For example, one radiologist at Hospices Civils de Lyon in France said that whereas he previously spent minutes on contouring, that now takes him considerably less time with AI – freeing up time for interpretation and patient interaction.
Turning imaging data into insights with AI-enabled analysis
Beyond segmentation, AI is transforming how imaging data is interpreted and acted upon. By analyzing vast volumes of medical imaging data in seconds, AI tools can surface patterns that might otherwise go unnoticed, complementing the power of the human eye and reducing the cognitive burden on radiologists. In lung cancer screening, for example, early detection is vital for improving patient outcomes. AI-assisted analysis can help radiologists identify lung nodules 26% faster and detect 29% of previously missed nodules. In emergency settings, AI systems can automatically flag radiography scans that show no immediate signs of bone fracture, helping triage patients more efficiently and enabling radiologists to concentrate on the most urgent or complex cases.
2. Deep workflow integration: embedding AI systems into clinical practice
While addressing real human needs is the foundation of effective AI in radiology, its clinical usefulness ultimately depends on seamless integration into daily practice. Even the most advanced AI solutions can fall short if they add friction rather than remove it. Radiologists consistently emphasize that they want AI systems embedded within their existing diagnostic workflows, not a proliferation of separate apps that make work more complicated for them.
Seamless integration for faster, more confident diagnosis
That kind of deep integration is already becoming a reality in leading radiology departments. By collaborating closely with clinicians during the development, validation, and implementation of new AI solutions, we can ensure these tools fit naturally into existing workflows. For example, at Fundação Instituto de Pesquisa e Estudo de Diagnóstico por Imagem in Brazil, radiologists can now view AI-generated insights directly within their diagnostic viewer. Chest X-ray turnaround times have dropped to as little as two minutes, supporting faster, more informed and confident decisions.
Building open ecosystems to advance radiology AI
While examples like this show what’s possible when AI is deeply integrated into existing workflows, many providers are now grappling with a broader challenge: how to scale that integration across an entire health system. Many rely on multiple AI tools for tasks ranging from nodule detection and organ segmentation to triage and reporting. Without coordination, these separate point solutions risk creating fragmented workflows, increasing IT burden, and complicating governance. An open, interoperable approach is essential to address these challenges. By connecting different AI applications and clinical data through integrated platforms, healthcare providers can embed them into existing workflows more easily. Such open ecosystems can also make it easier to integrate emerging AI algorithms and models, thereby accelerating innovation.

3. Building trust in radiology AI: the missing human link
In addition to human-centered AI that integrates seamlessly into the workflow, trust has emerged as the third – and arguably most critical – pillar of adoption. If radiologists don’t trust AI, they won’t use it. And that trust is not a given. Despite high optimism, concerns remain. Our 2025 Future Health Index shows that 63% of radiologists are concerned about bias in AI algorithms, and an equal proportion worry about who holds legal liability when using AI. Without clarity on these and other issues, even validated AI tools may face skepticism or resistance.
Earning radiologists’ trust
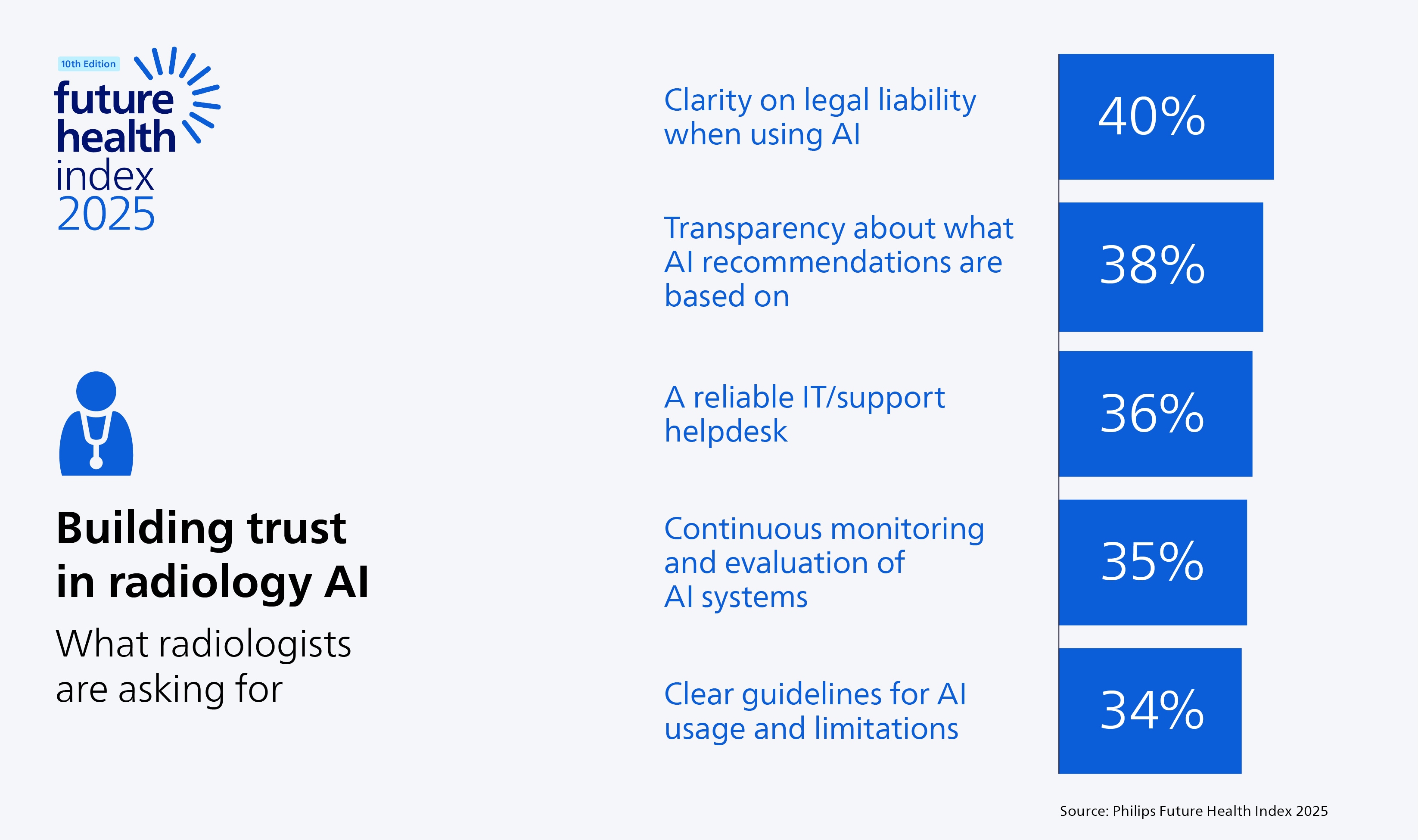
What can help build trust among radiologists? The 2025 Future Health Index highlights several key factors. The most prominent is clarity on legal liability when using AI (40%), followed by transparency about what AI recommendations are based on (38%) and having a reliable IT/support helpdesk (36%). In addition, ongoing monitoring is essential to continuously assess AI’s safety and effectiveness in real-world clinical settings after implementation. Radiologists also want clear guidelines for AI usage and clarity about its limitations. Beyond transparency, strong governance frameworks are important. Hospitals are increasingly recognizing the importance of setting up AI oversight boards to review model performance, including potential model drift over time, monitor for possible bias, and ensure ongoing compliance with regulatory standards. Such governance frameworks mirror existing quality assurance programs that radiologists already trust, expanding the reach of these types of programs beyond human performance to machine performance as well.
Extending trust to referring physicians
AI in radiology affects not only those who interpret images, but also those who act on them. Referring physicians depend upon imaging reports to guide diagnostic and treatment decisions, making their confidence in AI-supported results equally critical.Research shows that referring physicians are more likely to trust AI when its outputs are transparent, legal responsibilities are clearly defined, and strong data protection measures are in place [5]. Meeting these expectations is essential to enable responsible adoption, build trust, and ensure the effective integration of AI into clinical radiology workflows.
Building patient trust in AI
Trust must also include patients. While 85% of radiologists in the 2025 Future Health Index express optimism about AI in healthcare, only 59% of patients feel similarly confident. Their trust varies depending on the task: patients welcome AI for administrative processes like scheduling or triage but remain cautious about its role in clinical decision-making. Our research shows that patients are looking for reassurance that AI improves care quality, protects their data, and gives clinicians more time to listen to them. Interestingly, patients prefer to receive information about AI from their own doctors. That finding underscores the central role of radiologists in communicating about AI and guiding patients through its use. Transparent communication also means offering choices where possible. For example, digital triage systems could allow patients to choose between an AI-assisted consult for faster guidance or a traditional in-person visit. Giving patients agency in how AI is applied could reinforce trust and reassure those with lingering concerns.
The future of AI in radiology: from assistive to agentic AI systems
Taken together, the three factors we discussed – putting people first, integrating AI seamlessly into workflows, and building trust from all involved – form the foundation for effective and responsible adoption of AI in radiology. But the possibilities don’t end there. As AI in radiology continues to evolve, innovation is moving beyond narrow, task-specific tools toward agentic AI systems that can support radiologists across the entire workflow. Rather than executing isolated tasks, agentic AI systems will learn from radiologists’ behaviors and preferences to deliver more adaptive, context-aware support. These systems could, for example, personalize imaging protocols, prioritize urgent cases, and surface the most relevant information at the right moment, serving as intelligent collaborators that enhance both efficiency and diagnostic confidence. Looking toward the future, we’ll also see continued progress in multimodal AI systems and integrated diagnostics. AI can help combine data from multiple imaging modalities and other clinical sources – such as pathology, genomics, and laboratory results – to provide a more comprehensive analysis of each patient and their disease progression. In cancer care, for instance, integrating radiology, pathology, and lab data into a single view can help care teams collaborate more effectively. Such multimodal insights can support more precise and personalized treatment planning. That future can only be built in collaboration. To fully deliver on the promise of AI-driven radiology and integrated diagnostics, we must bring together AI developers, data scientists and medical professionals. Each offers vital expertise and a unique perspective. But no one can succeed alone. By developing solutions close to where radiology is practiced, always with human needs at the center, we can foster innovation that truly improves the lives of radiologists, care teams, and patients. To discover what’s next in AI in radiology and learn more about how Philips is helping customers advance AI-powered precise diagnosis, join us at RSNA 2025.
Sources [1] American Journal of Roentgenology, 2024 – Best practices: burnout is more than binary. https://doi.org/10.2214/AJR.24.31111 [2] Philips Future Health Index, 2024. https://www.philips.com/c-dam/corporate/newscenter/global/future-health-index/report-pages/experience-transformation/2024/first-draft/philips-future-health-index-2024-report-better-care-for-more-people-global.pdf [3] Artificial intelligence in medical imaging, 2024 – Understanding the factors influencing acceptability of AI in medical imaging domains among healthcare professionals: A scoping review. https://doi.org/10.1016/j.artmed.2023.102698 [4] European Radiology, 2020. Implementation of artificial intelligence (AI) applications in radiology: hindering and facilitating factors. European Radiology. https://doi.org/10.1007/s00330-020-06946-y [5] Insights into Imaging, 2025. Implementation of AI in radiology: the perspective of referring physicians. https://insightsimaging.springeropen.com/articles/10.1186/s13244-025-02120-4








