10 real-world examples of AI in healthcare
Nov 24, 2022 | 7 minute read
Artificial Intelligence (AI) has burst onto the scene in healthcare in recent years, giving rise to new innovations that promise to improve patient health outcomes and workflow efficiencies. From diagnosis to treatment and home care, AI has shown potential to support healthcare professionals and patients at every stage of the care continuum. Here are 10 real-world examples of AI in healthcare, showing how it can enhance experiences for patients and staff alike.

1. Improving precision in patient positioning and CT image reconstruction
Radiology departments continue to face challenges in terms of increasing patient volumes and ensuring consistency in image quality, while at the same time improving operational efficiency. With Computed Tomography (CT) being one of the most widely used imaging modalities, radiology departments have a lot to gain from AI-enabled solutions that help streamline CT workflows and maximize image quality. That starts with getting a patient in the right position for an exam. In CT, patient mispositioning is a common challenge, which can result in increased radiation dose to the patient or image noise [1]. AI-enabled camera technology can automatically detect anatomical landmarks in a patient to enable fast, accurate and consistent patient positioning. In addition, AI-enabled image reconstruction can help to reduce radiation dose and improve CT image quality, thereby supporting diagnostic confidence.

2. Speeding up image acquisition in MR
Magnetic resonance (MR) is another imaging modality that plays an ever-more important role in precision diagnosis of medical conditions. The rising use of MR is increasing the pressure to efficiently scan more patients and to shorten the path from initial scan to final diagnosis. At the same time, MR departments are looking for ways to improve satisfaction of patients and referring physicians. Enter AI-based image reconstruction, which can accelerate MR exams to increase department productivity and reduce the cost per exam, while supporting diagnostic confidence with high-resolution images. On top of that, the technology increases MR accessibility for patients who are stressed, anxious or in pain. Because it shortens exams and provides first-time-right scans regardless of patient condition, patients spend less time in the scanner, thereby improving their experience.

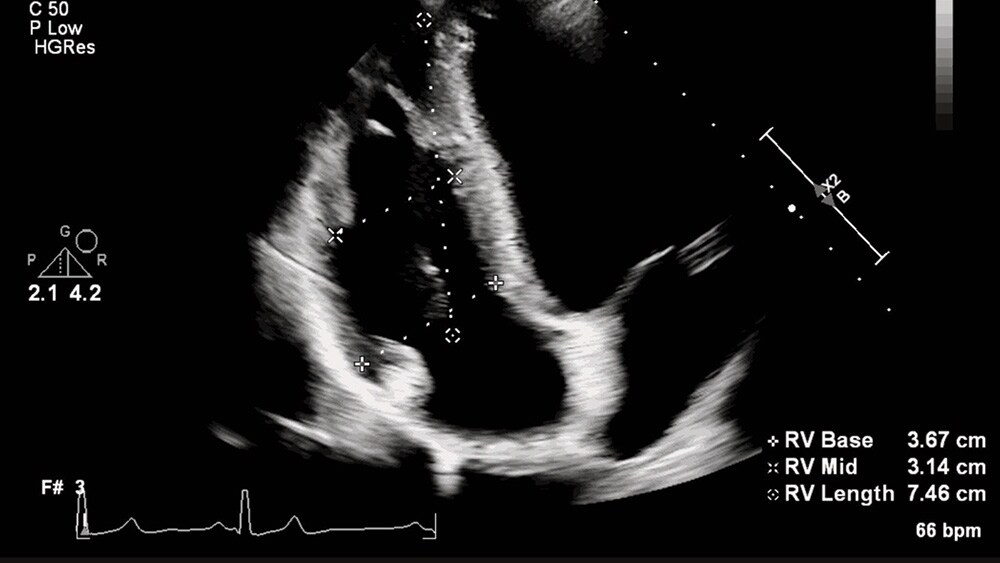
3. Taking the complexity out of ultrasound measurements
In cardiac care, ultrasound has developed into an indispensable tool to help visualize and evaluate a patient’s heart function. In fact, it is now often the first imaging modality used to diagnose patients [2]. However, the challenge with ultrasound is that it strongly relies on the person operating the system. Certain measurements, which are needed for every echo exam, can be time-consuming and have high inter- and intra-user variability. With AI, we can take away some of that manual and repetitive labor; just like in some of the other AI in healthcare examples in this overview. AI-based automatic measurements can deliver fast and reproducible echo quantification, improving both the patient and staff experience. Healthcare professionals can accept or modify measurements based on their own clinical assessments, giving them a powerful tool to enhance their expertise while remaining in control of diagnostic decision-making.
4. Helping radiologists read images faster and more accurately
Similarly, AI can support with image segmentation and quantification in radiology, thereby enabling radiologists to focus on higher-level interpretation of images. AI can also act as a second set of eyes, serving as an adjunct to the radiologist’s decision-making by pointing them to areas of interest or incidental findings they may have overlooked. For example, AI algorithms that scour MR images of the brain for subtle neurological changes over time have been shown to improve diagnostic accuracy in multiple sclerosis patients by 44%, while reducing reading times [3]. Similarly, AI-based lung nodule detection can perform nodule search 26% faster, detecting 29% of previously missed nodules compared to manual inspection [4]. For time-pressured radiologists who have to interpret more images than ever before, such AI-enabled support can make a meaningful difference, while also benefiting the patient.

5. Supporting multidisciplinary collaboration in cancer care
Beyond analyzing single sources of data, there are also examples of AI in healthcare that show it can help connect previously disconnected and disparate patient data – providing novel insights that support healthcare professionals in their decision-making. In cancer care, for example, AI can help integrate information across different clinical domains such as radiology, pathology, EHR systems, and genomics – providing a clear, intuitive view of the patient’s disease state. This can assist multidisciplinary tumor boards in making timely, informed treatment decisions, to give every patient the best chance of a positive treatment outcome. In the future, the intelligent integration of data could give further insight into a patient’s prognosis, supporting selection of the best care pathway for that particular patient based on an analysis of treatment outcomes for similar patients.

6. Guiding physicians during minimally invasive surgical procedures
Interventional physicians, who perform minimally invasive procedures on patients with heart disease and other conditions, are another group to gain from AI-based workflow automation and clinical decision support. For example, in stroke care, cloud-based AI can help analyze CT images to automatically detect large vessel occlusion – a major source of stroke – as well as its location. The software then shares this analysis with physicians at the primary stroke center and at the intervention center where the patient is eventually treated. Similarly, cloud-based AI can aid in planning and guiding endovascular surgery, helping interventional physicians to operate more accurately and efficiently.

7. Detecting early signs of patient deterioration in the general ward
In acute and post-acute settings, there are similar examples of how AI in healthcare can enhance the human experience. Almost 1 in 5 patients in medical-surgical areas of hospitals will experience postoperative serious adverse events [5]. Manual checks of vital signs can be time-consuming and are subject to human error. By automatically monitoring vital signs and calculating early warning scores that signal possible patient deterioration, AI-enabled tools can help nurses and care teams identify early signs of events such as respiratory failure or cardiac arrest, allowing them to respond rapidly. In doing so, one hospital managed to reduce serious adverse events in the general ward by 35% and cardiac arrests by more than 86% [6].

8. Minimizing equipment downtime through predictive maintenance
Next to augmenting the skills of physicians and staff, AI can also help improve continuity of care by predicting when medical equipment is in need of maintenance. For example, through remote sensing, we can monitor and analyze over 500 parameters on an MR machine, allowing us to identify proactively when certain hardware parts may need maintenance or replacement. As a result, 30% of service cases can be resolved before downtime is caused – preventing avoidable interruptions to clinical practice and unnecessary patient delays [7]. In the future, having a full digital twin, or virtual representation of an entire imaging fleet, could allow for even more comprehensive predictive maintenance and continuous operational optimization.

9. Forecasting and managing patient flow to streamline hospital operations
On an enterprise level, AI can help manage and optimize the utilization of equipment, beds, and staff by providing predictive insights. With hospital resources being increasingly strained, the ability to anticipate and adapt to rapidly changing circumstances has become more essential than ever. Using the power of AI, we can extract relevant patterns from vast amounts of real-time and historical hospital data to forecast and manage patient flow. This generates actionable insights that can help answer questions such as: which patient should get an intensive care bed first? Or: which patient is ready to be transferred to a stepdown unit? Having such insights at their fingertips enables healthcare providers to get the most out of precious resources and manage transitions of care more effectively, from admission to discharge – ensuring that every patient gets the right care in the right place at the right time.

10. Monitoring cardiac patients remotely for timely diagnosis and care
As healthcare increasingly moves from the hospital into the home and the community, the power of AI doesn’t remain confined to hospital walls. It can also be applied to data that is conveniently collected at home or elsewhere, through medical-grade wearable technology. For example, in cardiac care, cloud-based AI can help with the quick detection of atrial fibrillation or heart rhythm disturbances, based on an analysis of remote electrocardiogram (ECG) recordings. Atrial fibrillation affects millions of people each year. However, the condition is often unrecognized and untreated. By flagging readings that may require the most urgent attention, clinicians are empowered to deliver cardiac care faster and more efficiently. With AI-assisted analysis, cardiac care could eventually become more predictive and proactive. A recent study underscored this potential, showing how a deep learning model can predict the short-term risk of atrial fibrillation based on 24-hour Holter recordings [8]. It’s yet another example of how AI can help improve patients’ lives, by getting them the care they need sooner.

Read more about other AI in healthcare examples
Download our position paper How AI can enhance the human experience in healthcare
Sources [1] Habibzadeh MA, Ay MR, Asl AR, Ghadiri H, Zaidi H. Impact of miscentering on patient dose and image noise in x-ray CT imaging: phantom and clinical studies. Phys Med. 2012;28(3):191 199. https://pubmed.ncbi.nlm.nih.gov/21741870/ [2] From discussions with users of Philips ultrasound technology. American Society of Echo, EACVI, Klein reports. [3] Based on (a) a publication from European Radiology 2019 (University of Cologne) - Follow-up MRI in multiple sclerosis patients: automated co-registration and lesion color-coding improves diagnostic accuracy and reduces reading time; and (b) ISP 9 Philips whitepaper: The clinical utility of a novel imaging application for serial brain imaging: MR LoBI. [4] Lo, SB, Freedman, MT, Gillis, LB, White, CS, and Mun, SK. American Journal of Roentgenology 2018 210:3, 480-488. https://www.ajronline.org/doi/full/10.2214/AJR.17.18718 [5] Bellomo R, Goldsmith D, Russell S, Uchino S. Postoperative serious adverse events in a teaching hospital: a prospective study. Med J Aust. 2002: 176:216-218. [6] https://www.philips.com/a-w/about/news/archive/case-studies/20180315-early-warning-score-reduces-incidence-of-serious-events-in-general-ward.html [Results are specific to the institution where they are obtained and may not reflect the results achievable at other institutions] [7] The future of healthcare is smart and connected: a vision for digital transformation. https://www.philips.com/a-w/about/news/archive/blogs/innovation-matters/2021/20210614-thefuture-of-healthcare-is-smart-and-connected-a-vision-for-digitaltransformation.html
Share this page with your network