Philips presents symposium on remote patient monitoring of COPD patients at ERS International Congress 2020
The European Respiratory Society (ERS) held its virtual International Congress 2020 from September 7-9, where Philips presented two clinical symposia, each touching on a different aspect of home ventilation and patient management. One of those symposia focused specifically on the evolving role of telemedicine in initiating home non-invasive ventilation (NIV) for COPD patients, featuring expert speaker Dr. Marieke Duiverman, Department of Pulmonary Diseases/Home Mechanical Ventilation, University Medical Center Groningen, The Netherlands. Dr. Duiverman has been conducting research around the use of telemedicine in initiating home non-invasive ventilation (NIV) in stable hypercapnic COPD patients in The Netherlands, and discusses the implications for both patients and providers, as well as the overall healthcare system. Just before the show, Philips sat down with Dr. Duiverman to learn more about her research and how she sees the role of telemedicine changing the respiratory care industry.
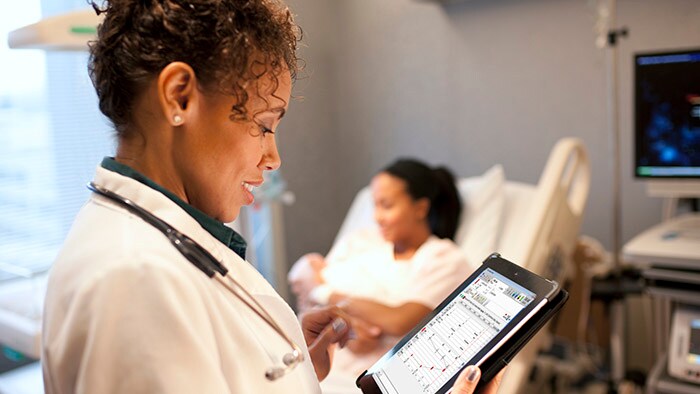
Q. How have you seen the use of home NIV evolve over the years? What does adoption and impact of telemedicine and home NIV look like market-to-market? A. Over the last 20 years, the use of home NIV has evolved quite significantly, especially when compared with standard care. In the past, NIV therapy for the COPD population was not commonly prescribed in the Netherlands, but our study published in 2008/2011 showed positive results and additional trials proved greater efficacy. Although we are steadily moving forward with home initiation of NIV therapy, many hospitals are still sticking to what they have always been used to – in-patient hospital initiation. We are currently seeing an evolution, however. More and more patients are in search of these newer treatments and are more eager to receive treatment at home. The onset of COVID-19 has certainly forced us to speed up implementation of home initiation to free up hospital beds faster than before and keep COPD patients from visiting the hospital unnecessarily during the pandemic. We certainly see a range of differences in the implementation of telemedicine and home NIV across Europe. Many of the issues stem from an organizational standpoint and how reimbursement systems are set up in different countries. Currently, some clinicians and providers find it very difficult to move to a home-based system because of the reimbursement models that are in place, and find it more cost effective to treat patients in the hospital. In other areas, there is inadequate access to beds for elective patients so they must find a solution that allows them to administer care in the hospital during the day and then discharge patients overnight for home ventilation. Q. What would the process need to look like (initial steps, integration, ongoing monitoring, etc.) for a provider to initiate this method of treatment? A. Providers will need to first look at the organization of their teams to ensure that they can adequately administer remote care and monitoring. They’ll likely need more nurses, who will need to receive training. They’ll also need to ensure that their set-up is reliable and secure since there is a lot of data transfer taking place. The most important thing is to then identify the right patients for this to be successful. When starting such a service, you need to focus on those patients who would most benefit. A lot of this will improve over time, but initial conversations with patients will help clarify their motivation and commitment. And, of course, setting clear goals and outlining expectations on how they may improve with this type of treatment is vital. Patients should be made aware that homecare treatment can be just as effective as in-hospital management, in an environment that may be more convenient and comfortable, where they can also expect to see improvement in fatigue, sleep and so on. Providers should also consider investing in remote monitoring capabilities to track the vent data and monitor CO2 levels. They’ll definitely want to see that the ventilation is improving so that clinicians can have oversight of this and alter treatment where necessary.
Q. What are the biggest challenges and/or insights of which providers should be aware? A. COPD is a progressive disease that can ultimately reduce the quality of life for the patient, so they are undoubtedly anxious about receiving treatment, especially if we need to start them on high intensity NIV therapy. When implementing telemedicine and home NIV initiation, there are a number of considerations that providers need to keep in mind: There are also political and geographical challenges to consider. In some regions, the application of care is entirely dependent on organizational structure and reimbursement. Many countries do not reimburse for elective or home care, while some countries don’t have enough hospital beds to support elective patients and have no other choice but to find creative solutions to discharge patients and treat them at home. It tells us that homecare will never be a primary practice. Patients will always need more guidance and organizational structures will always vary. But as the world begins to become more aware of alternative chronic respiratory treatment options, perhaps broader organizational reimbursement will follow. Q. What results have you seen in your research from initiating home ventilation using remote monitoring/telemedicine? A. In talking with our patients, we continue to learn that most do not want hospital care, and prefer to begin with NIV initiation at home, where they feel most comfortable. For those that are more debilitated or disabled from the disease, the need for home NIV increases greatly. With more flexibility on how to organize care in the home, caretakers can provide a level of comfort and support, lessening any anxiety patients may be feeling about receiving treatment. Via our non-inferiority study of COPD patients, we found that it was as equally effective to start at home, where many of the outcomes remained the same, with costs dropping by at least one third. Before these studies began, it was assumed that home ventilation for COPD patients was impossible due to their need for higher pressures and more frequent pressure adjustments. But through our research, we found that it was not only possible, but in many cases just as effective and less expensive. Our ultimate goal is to improve the overall quality of life for the patients, so providers will need to assess each patient’s individual circumstances and any comorbidities involved to be clear about the disease, and work to tailor their therapy to their unique situations. To follow along with Philips presence at ERS 2020 Congress or watch the symposia on demand, login to our Philips ERS experience using your virtual show badge.

Share on social media
Topics
Contact

Meredith Amoroso
Philips Global Press Office Tel: +1 724-584-8991
You are about to visit a Philips global content page
Continue