The hospital of the future is not a physical location with waiting rooms, beds and labs. It will instead be a network with nodes and connections. Technology, in other words, will be the starting place of our new spaces and will allow us to approach health and care in new ways. A good example is Mercy Virtual Care Center, the $54 million, 125,000-square-foot facility which has no patients on-site. It has over 300 medical professionals who sit in front of what looks like a trading desk or flight control station. They are taking care of patients at home and in beds in 38 hospitals in seven states.
Access means one-mile, one-click, one-call – anytime, anywhere
In thinking about the design for care that keeps people healthy, rather than only treating someone who is sick, we need to build a healthcare system that is connected, aware and adaptive to patient needs. One that allows for continuous monitoring of patients anywhere, so that care is provided wherever and whenever it’s needed. This means retail-type outlets close to where people live, specialist hubs, in-patient facilities, out-patient clinics and ambulatory patients (or rather health consumers), all connected into a single network. It reminds me of what we worked on at Citibank 20 years ago: Access means one-mile, one-click, one-call: an around-the-clock, anytime, anywhere network, with a physical outlet within one mile in urban areas, one click on an app or one call away. We can see this shift happening with the consolidation of care in the U.S and the emergence of Integrated Delivery Networks. Hospitals are becoming holistic networks that work with labs, clinics, primary care practices and other providers in a system that’s required to keep communities healthy. Already, there are examples of how the connected network approach might improve both the consumer experience as well as the outcomes we are able to achieve. Through a partnership between Philips and Banner Health, one of the largest nonprofit health systems in the U.S., we have seen a nearly 50 percent drop in hospital admissions by leveraging telehealth for patients with multiple chronic conditions. The telehealth program utilizes clinical software and in-home IoT monitoring devices, allowing regular interaction with caregivers helping patients build self-care skills, either through two-way video or face-to-face. With a well-connected multidisciplinary care team, smart devices for monitoring, advanced analytics doing their work behind the scenes, we are able to put together a complete picture of the patient. One that gives full context, spots changing patterns in behavior and/or health at an early stage. This enables the care team to address issues efficiently before a hospital stay is needed. The care for high-intensive users of healthcare obviously carries significant healthcare costs. Five percent of the chronically ill patients account for up to 50 percent of all healthcare spending. Now several years into the program, Banner has reduced overall cost of care by over 34 percent, according to the latest study.
We will need to reimagine our physical spaces – both from a technology as well as a design perspective
It has also become clear that for the hospital of the future, we will need to reimagine our physical spaces – from a technology as well as a design perspective – with both the patient and the caregiver perspectives in mind to better integrate care into end-to-end care flows. Hospitals are still mostly organized around acute care and medical silos. While size of sensors is decreasing, their sensitivity is increasing exponentially. With chips holding ever more computing power, soon even the smallest devices will be capable of storing artificial intelligence capabilities onboard, making them more personalized, intuitive and aware. Together, the growing adoption of cloud technologies and the rise of 5G will play a role in this transformation, as hospitals will rely on high fidelity, data-rich monitoring – either built directly into the rooms or through home devices to monitor remotely. These smart devices will feed large amounts of patient data to providers in real time, which requires a fast and capable network. Driving the adoption of 5G is one of Philips’ goals in partnering with Qualcomm, who already are bringing virtual reality and AI-enabled chip sets to devices. When you take these technological advancements into account and you apply design thinking principles, you can sketch ambient intelligent environments that anticipate user needs with the ultimate goal to augment the patient’s capabilities and provide a seamless experience across the full health continuum: from prevention to diagnostics, treatment and home care, but also from the very start of life to when we are old.

An example is a Philips design concept that supports a woman and her partner during labor with monitoring and interactive lighting animations, an app and EMR data integration. This creates a better labor and delivery experience for women giving birth in the hospital. This visualization grows and changes in response to physiological data obtained by contraction monitoring, and is combined with a labor breathing guide that provides the woman with timely support to cope with contractions.

Another example is the NICU (neonatal intensive care) concept that takes a connected family-centered approach to caring for the most fragile among us, the prematurely born, with the aim to anticipate their very personal and highly specific 24/7 needs, both clinical and mental, in the crucial development period after being born. The key is to take a design approach in an open ecosystem capable of embracing and enabling a true end-to-end patient journey, versus silo-ed, disconnected point-solutions. In a digital hospital the patient is truly at the center of the network. Imagine a stroke patient for whom every second counts. An elderly patient is at home, wearing a Philips Lifeline pendant, with a tiny built-in mobile phone. The patient has a stroke and falls. Automatically the 24/7 response center is alerted, the patient profile, which includes her medical history, and vital signs are analyzed. The right ambulance is ordered. En route, high-res images are captured by a portable CT scanner to locate the clot. Patient data streams to the hospital ahead of the patient’s arrival. Upon arrival, the patient is immediately rushed into treatment, using smart catheters to remove the clot, guided by augmented reality.
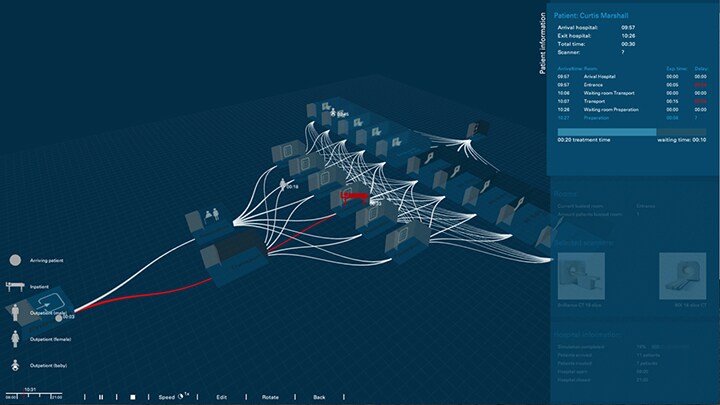
The patient is then moved to ICU where devices such as monitors, lights and ventilators automatically adapt to the patient. The patient is remotely monitored by the eICU command center. Based on the information from the monitors and patient profile, the right time of discharge is determined. The patient gets a tiny biosensor in a patch that she wears for a couple of weeks. And at home the patient is now continuously monitored. Stroke survival is highly time critical. With the Internet of Medical Things and cloud-based data aggregation and analysis, we will improve outcomes and survival rates for the millions who suffer strokes annually. We will create deep patient profiles that contain longitudinal data from multiple sources, in increasing granularity and frequency. The profiles allow for highly relevant, actionable information supporting patients, caregivers and clinicians alike, and will combine data from medical records, biopsies, biome, digital pathology and genomics, as well as patient-generated data from wearables and apps. Of course, challenges remain as to how we realize this vision. The first is that we need to overhaul the existing incentives, like fee-for-service, so that we encourage care based on quality and outcomes. The second requires an even bigger transformation: working in a multi-disciplinary, collaborative way and augmenting people with technology. If we can build physical and virtual spaces that incorporate patient-centricity and human touch we will create systems that drive better health outcomes at lower cost. This article was previously published by Jeroen Tas on his personal Linkedin profile and updated on 10 September 2019.
Share on social media
Topics
Author

Jeroen Tas
Chief Innovation & Strategy Officer Jeroen is an experienced global executive and entrepreneur with a track record of leading innovation in the healthcare, information technology and financial services industries. Leading the company’s global Innovation & Strategy organization, he’s responsible for creating a pipeline of innovative business propositions that address emerging customer needs and enable a high-growth, profitable health continuum strategy.
Follow me on













