When I joined Philips almost 35 years ago, open heart surgery was the norm for treating conditions such as coronary artery disease. A patient would spend more than a week in the hospital. Today, a patient treated for coronary artery disease is often able to walk out of the hospital the same day – thanks to the development of minimally invasive procedures. It goes to show how image-guided therapy has revolutionized surgical procedures over the past few decades, and as Chief Business Leader for Image Guided Therapy at Philips, I couldn’t think of a more rewarding field to be in. But as I meet with clinicians and healthcare leaders around the world, listening to their needs, dreams and concerns for the future, it also becomes clear that what got us here won’t get us there. Together, we are really just at the beginning of a much longer innovation journey. As hospitals are pressed to do more with less, new solutions are needed to deliver improved care to more patients, while reducing costs, easing the burden on overstretched staff, and at the same time improving patient experience. In other words, what we call the Quadruple Aim. Looking at the future of image-guided therapy, I see particular promise in five exciting areas of innovation that can help deliver on this Quadruple Aim.
1. Artificial intelligence – a smart assistant in the interventional suite
One of the biggest challenges in the interventional suite I hear from clinicians today is the sheer amount and complexity of data they acquire every day, and the difficulty in deriving meaningful insights from it. This is where artificial intelligence (AI) holds tremendous promise. With its ability to sift through and extract actionable insights from large amounts of data, AI offers new ways to provide clinical decision support and speed up workflows. First of all, AI could help to alleviate the mounting administrative burden in the interventional suite, allowing clinicians to focus more on the procedure and the patient. Administrative work is widely recognized as a major source of professional burnout in healthcare, and interventionalists are no stranger to it. After treating six to eight patients in one day, having to spend another two hours on reporting can easily wear you down.
AI could help to alleviate the mounting administrative burden in the interventional suite, allowing clinicians to focus more on the procedure and the patient.
With AI, we now have the tools to start automating this process. Suppose we use AI to automatically track each step of a procedure, log relevant events and actions, and then auto-populate reports with images and measurements acquired during the procedure. A clinician would only have to review, complete, and sign off the pre-populated report at the end of procedure. This could make a big difference to both the clinician and the patient: every minute saved on reporting is a minute gained to interact with the patient.

I foresee that AI will also take on a growing role in providing real-time clinician decision support in the interventional suite. With minimally invasive procedures, every millimeter matters – especially in the most critical areas of the body such as the heart. Computer-assisted interpretation of images could go a long a way in further improving accuracy, offering a helping hand to the clinician. Already today, there are advanced methods to automatically recognize anatomical structures of the heart, based on ultrasound images. In the long run, AI could also help to stratify patients to offer them the therapy with the biggest chance of success. For example, based on large historical data sets, AI may able to calculate the risk of bleeding or other complications during a procedure, depending on patient characteristics. Such a personalized, data-driven approach could help to improve outcomes, reduce complications, and drive down costs.
2. Augmented reality – a new way of looking at image-guided therapy
A second innovation area in image-guided therapy that offers immense opportunity is augmented reality (AR). With AR, we will be better able to address another common challenge reported by clinicians in the interventional suite: the need for increased flexibility to move around the patient during a procedure, while still having all relevant patient information in direct view. This is particularly relevant in procedures such as endovascular repair of aortic aneurysms, where clinicians enter catheters into the body from both sides of the table, while they have to pay attention to X-ray images on a monitor that is on one side of the table. Imagine having that same information right in front of your eyes, in a 3D hologram, without having to turn your head. That is the promise of AR.

Earlier this year, we announced a collaboration with Microsoft to pioneer the use of AR in image-guided therapy, combining Philips Azurion with the Microsoft’s HoloLens 2 holographic computing platform. This joint innovation allows the clinician to keep his or her eyes on the patient, while superimposing live data and 3D medical imagery needed to guide precision therapy. Clinicians will be able to fetch data and perform actions with eye tracking, voice control, and hand gestures – creating a personalized ‘cockpit’ that allows them to focus on the patient.
Augmented reality allows the clinician to keep his or her eyes on the patient, while superimposing live data and 3D medical imagery needed to guide precision therapy.
Although still work in progress, it’s easy to see how tools like these could help clinicians navigate through anatomical structures more accurately. This could have a real impact on quality and efficiency of care, as well as staff experience. Training, education, and remote assistance are other potential applications of AR. What if you were able to follow a procedure in real time through the eyes of a colleague, and offer specialist advice where needed? It sounds futuristic, but with AR this could eventually turn into reality.
3. Photorealistic 3D ultrasound – for enhanced procedural navigation
One source of 3D imagery that is already available in the interventional suite today is 3D ultrasound, which gives clinicians a much more intuitive understanding of anatomical structures than 2D images. Add to that the ability to generate 3D ultrasound images live and to fuse them with X-ray images in real time, and a moving organ like the heart becomes much easier to navigate because you can now see exactly where your devices are during a procedure.
We now have the ability to create live photorealistic renderings of anatomical structures.
One exciting development in 3D ultrasound, with great promise for the future of image-guided therapy, is that we now have the ability to create live photorealistic renderings of anatomical structures using a technology called TrueVue. The images below show the amazing level of detail in prenatal ultrasound images of an unborn child. It’s like peeking inside the body with a high-resolution camera.

With our latest imaging systems, we have started bringing this technology into the interventional suite for cardiac procedures – offering interventional cardiologists sharp and detailed 3D ultrasound images that help them navigate through the heart and get a better view of heart structures such as the mitral valves (shown below).
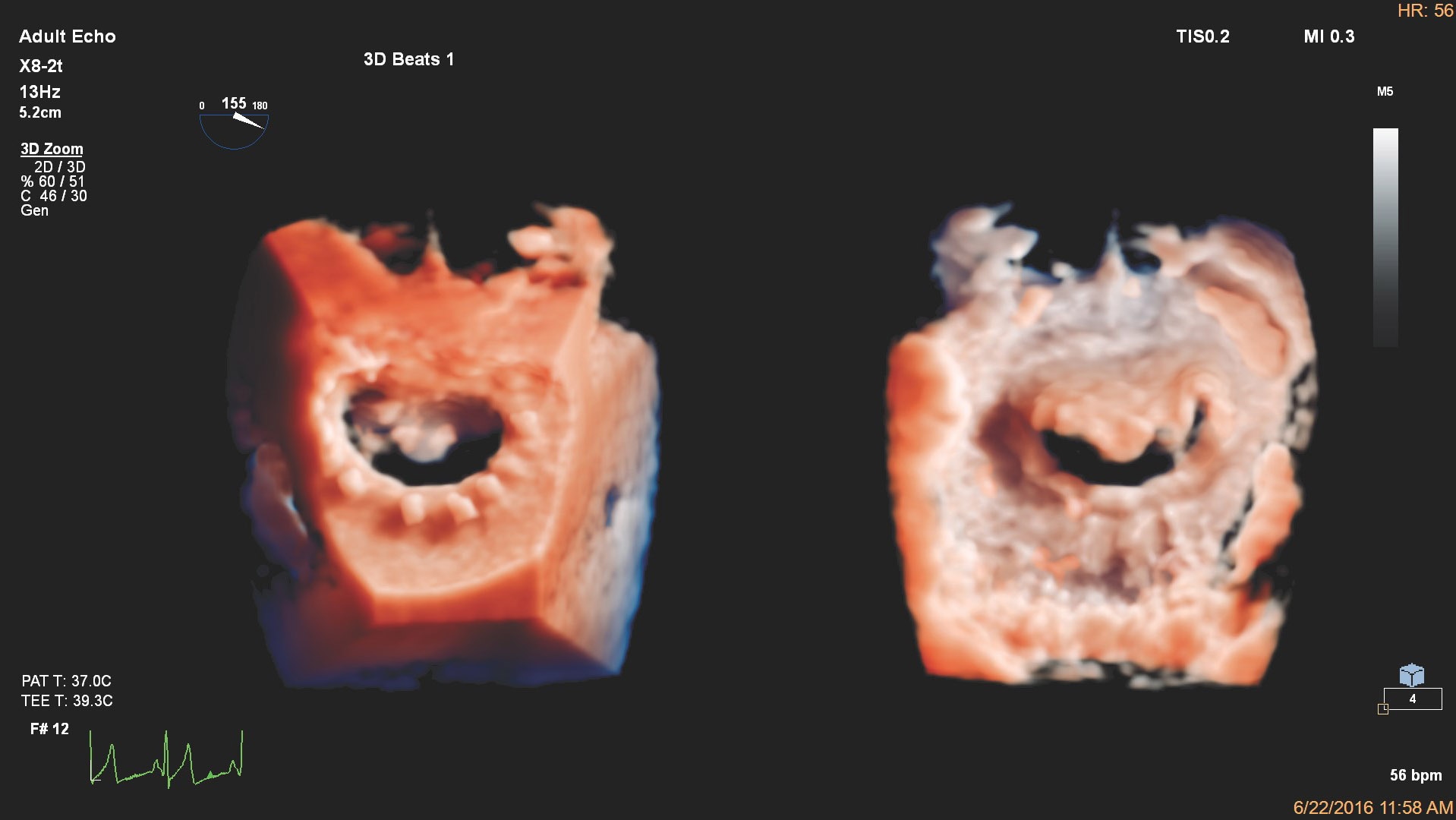
In the future, I envision that clinicians may increasingly be able to rely on photorealistic 3D ultrasound imaging applications for a wider range of procedures. Photorealistic rendering could also be applied to other imaging modalities, to further enhance procedural navigation.
4. Reducing the need for X-ray imaging – to minimize radiation exposure
Another important innovation area is minimizing radiation exposure by reducing the need for X-ray imaging. Over the last few decades, X-ray imaging is what has made many types of life-improving and often life-saving image-guided procedures possible. We need to be mindful, however, that X-ray dose levels should be kept as low as reasonably achievable to avoid harm to patients and staff. Fortunately, X-ray dose levels for most procedures have been significantly reduced already. For example, the dose of radiation received by interventional cardiology operators decreased by 95% between 2006 and 2017 [1]. We want to go further, however, and reduce the need for continuous X-ray imaging whenever possible.
We want to reduce the need for continuous X-ray imaging whenever possible.
For example, as I detailed in my previous article, in treatment of peripheral artery disease we can now take pre-operative CT and MR scans and overlay them on an X-ray image to create a 3D roadmap that guides the position of a catheter in real time. This reduces the need for additional X-ray imaging, limiting the burden on staff and patient.

Looking further ahead, I have high expectations of new, groundbreaking technology that could help clinicians visualize catheters and other intra-body devices in the context of the patient’s anatomy, from any possible angle, in real-time 3D – without having to step on the fluoroscopy pedal. Currently under research, this technology – called Fiber Optic RealShape (FORS) – uses pulses of light that run through hair-thin optical fibers. By analyzing how the light is reflected back along the fiber, we can reconstruct and visualize the full shape of devices. Eventually, this could reduce the dependency on X-ray fluoroscopy while allowing clinicians to see more during their procedures.
5. The integrated interventional suite – bringing it all together
With the introduction of new technologies into the interventional suite, procedures are becoming more and more advanced – but also increasingly complex. Clinicians need to collect and analyze information from a wide array of sources, such as live 2D X-ray images, 3D ultrasound, Intravascular Ultrasound (IVUS), and FFR or iFR physiological flow measurements. All while keeping an eye on the patient. That’s why innovation in the interventional suite is ultimately not driven by any single technology or imaging modality in isolation. Rather, it is the integration of different technologies and different sources of information that truly helps to innovate procedures. This was the guiding philosophy behind the development of our Azurion platform, which integrates many types of information at the patient table, and it continues to drive our innovations today.
Innovation in the interventional suite is ultimately not driven by any single technology or imaging modality in isolation, but by the integration of different technologies and modalities.
For example, earlier this year we launched IntraSight, which integrates intravascular ultrasound (IVUS) and FFR or iFR physiological flow measurements. Because different actions can be performed via the same table-side touchscreen, with various information sources brought together in one overview, clinicians no longer need to pull this information from different places or look in different directions – saving them time and effort.
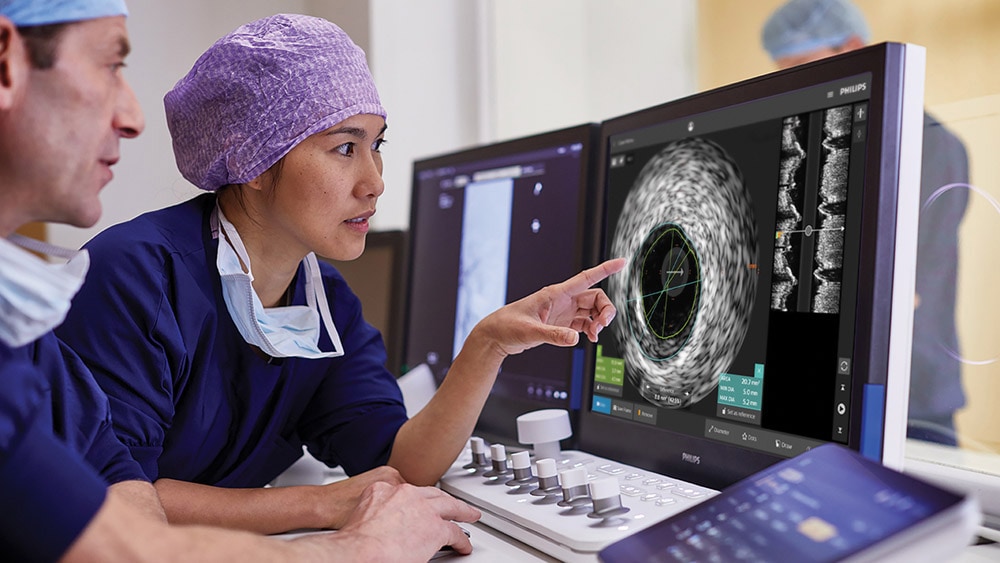
The ultimate vision is to create one seamless interventional suite; a place where all systems are connected and where the right information – compiled from different sources – comes to clinicians where and when they need it. But integration doesn’t end in the interventional suite. What if we could make it easier to reuse diagnostic imaging results for procedure planning, creating a seamless workflow from diagnosis and planning to intervention? What if, once the procedure is completed, we could streamline the export of results from the interventional suite to the EHR, PACS, and other hospital archiving systems, to ensure that the patient is followed up in the best possible way? Pursuing further integration across the entire patient journey has the potential to save time, reduce cost, and support seamless information exchange across settings.
Looking forward
Taking all of this together, I am incredibly excited how image-guided therapy will continue to break new grounds in the years ahead. In a truly integrated fashion, a wide range of innovations – from AI to AR and photorealistic 3D image rendering – will all help deliver on the Quadruple Aim: improved outcomes at lower cost, with improved patient and staff experience. Because ultimately, that’s what innovation in image-guided therapy is really all about. It’s not about technology per se. It’s about the patient who is about to undergo a life-saving procedure in the hope she will soon be able to go out for a hike with her loved one again. And it’s about the clinician who should have the time, tools, and intelligent support to take care of that patient in the best possible way. Reference [1] Faroux L, Blanpain T, Nazeyrollas P et al. Reduction in exposure of interventional cardiologists to ionising radiation over a 10-year period. International Journal of Cardiology, 2018; 259: 57-59.
Share on social media
Topics
Author

Bert van Meurs
Chief Business Leader of Image Guided Therapy, Chief Business Leader of Precision Diagnosis (ad interim) Bert van Meurs is Chief Business Leader of Image Guided Therapy, Chief Business Leader of Precision Diagnosis (ad interim), and is responsible for Diagnosis & Treatment. He is also a member of the Royal Philips Executive Committee.
Follow me on













