COVID-19 has turned nearly every aspect of patient care on its head, from supply chain logistics, to the comforts of human interaction. As COVID-19 rips through healthcare organizations globally, its wake can expose long-neglected workflow inefficiencies, care gaps, and the need for robust patient monitoring solutions and processes. Rightfully so, much of the COVID-19 conversation has focused on the lack of ventilators. However, any patient on a ventilator also needs to be on a monitor. Further, many other patients come to hospitals who don’t immediately need ventilator support, but do need some kind of patient monitoring. Those on the frontlines of this fight tell us how their organizations are stretched incredibly thin, many at the brink of their capacity if not already overflowing. On top of this, care teams are overworked, overwhelmed, and anxious about their own wellbeing and that of their loved ones. In order to maintain quality care while minimizing risk to staff, in-hospital monitoring solutions have played a pivotal role in achieving vigilant supervision of COVID-19 patients while limiting caregivers’ direct exposure to the disease. Here are four ways our customers are leveraging patient monitoring solutions to adapt to patient surges, maintain consistent visibility into patients’ health, and reduce clinicians’ infection risk.
1. Innovative approaches to scaling monitoring solutions
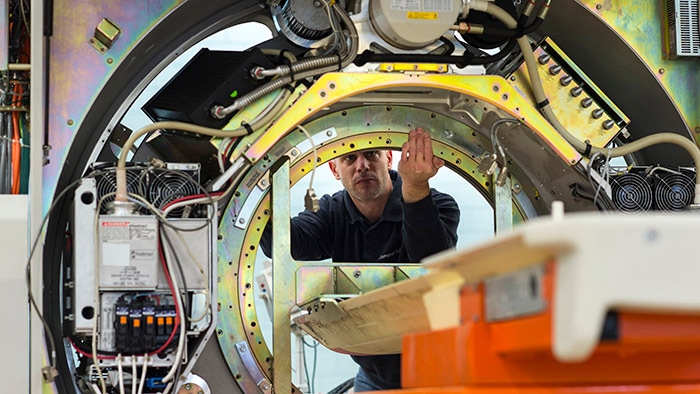
Many healthcare organizations are deploying innovative uses of existing monitoring solutions to get the most mileage out of them, and are even leveraging fetal monitors for non-acutely ill COVID-19 patients, or anesthesia machines for basic monitoring. In response to the surge in patient volumes, organizations are increasingly seeking monitoring solutions that can keep pace, adapt to specific needs, and integrate with other systems and devices to create central hubs for monitoring. As hospitals increasingly turn non-critical units such as ORs into ICUs, the staff may not have the training needed to monitor such acutely ill patients without the help of technology. Some organizations are integrating multiple patient monitoring views for solutions built for a single patient, or combining alerts from other systems to give care teams a comprehensive view of a patient’s health. There is a clear need for monitoring solutions that can expand outside of isolation rooms, to scale according to volume and to equip clinicians with meaningful, holistic vital sign data, while minimizing staff’s contact with the patient. Another way to scale ICU capacity is to leverage established best practices in remote monitoring. Frontline health systems, such as Northwell in New York, are sharing their recommendations for leveraging telehealth for the ICU in which patients are monitored remotely from a centralized, virtual care hub.
2. Uninterrupted care during patient transitions
With unlikely departments serving as pandemic units to help with overflow, patient transition periods can also result in gaps of essential data capture, such as respiratory rates, oxygen saturation, and changes in blood pressure. Hospitals are looking to transport monitors that are integrated with traditional monitoring, as the need for mobile, wireless monitoring systems is more critical than ever to ensure clinicians have visibility at every step of a patient’s journey. By achieving gapless data, these solutions prove to be vital for clinicians to have the most up-to-date, accurate portrayal of a patient’s health at their fingertips, especially for diseases like COVID-19 where a patient’s condition can quickly take an unexpected turn.
3. A renewed focus on early detection and real-time data
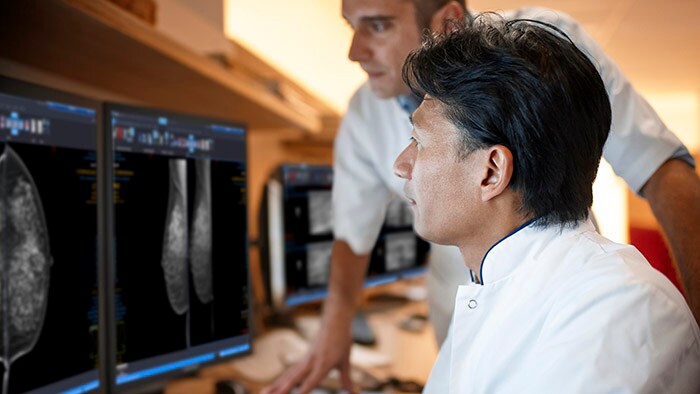
Additionally, we see far more emphasis placed on prevention and early detection. Clinicians need technologies that help triage and prioritize patient alerts, as well as help to reduce alarm fatigue and simplify workflows. For example, Early Warning Scoring (EWS) technologies produce a single benchmark that alerts clinicians if the patient is showing signs of distress, allowing care teams to intervene quickly and address health issues before they escalate. Such technology has also adapted to the specific needs of COVID-19 patients and key vital measurements needed, such as blood oxygen level measurements.
Because healthcare organizations are learning more about COVID-19’s transmission, symptoms, and recovery every day, real-time, holistic patient data is of the utmost importance. Frontline clinicians relay the importance of having easy access to medical history to understand each patient’s risk, especially for patients with comorbidities or compromised immune systems who have proved to be vulnerable to COVID-19. When monitoring a COVID-19 patient in the hospital, being on top of subtle changes in a patient’s condition and tracking trends over time could save the patient’s life, and the lives of patients that follow, as we learn more about this virus’s behavior.
4. Exploring contactless monitoring solutions
In the face of COVID-19, our customers’ priorities are to minimize staff’s contact with patients and medical devices, while continuing to care for COVID-19 patients to the best of their ability. However, many of them are faced with antiquated monitoring and rounding processes that require a significant amount of human interaction to deliver information. We have seen health systems adopt ways to limit staff exposure, such as running cords outside of patient rooms to monitors and IV pumps to eliminate unnecessarily exposure and reduce use PPE, or implement remote bed viewer solutions or use of remote controls. In the aftermath of COVID-19, I predict that we will see adoption of contactless monitoring solutions continue to grow, such as wearable biosensors or camera-based systems that can measure vitals, in an effort to offer clinicians an alternative to minimize infection risk. Beyond the monitoring needs that we are seeing for COVID-19 patients today, these tools will power care beyond the walls of a health system and establish a new normal for monitoring patients remotely, such as those with chronic conditions.
It takes a village
As we reflect on what we have learned from COVID-19 so far, we recognize the fight is not over, and there is much work to be done to support the scale-up of secure, connected, and intelligent monitoring that strengthens networks within health systems and beyond. We are eternally grateful for the frontline clinicians working tirelessly to prioritize the wellbeing of their patients, and the healthcare organizations creatively pivoting strategies to make the most of their limited resources. It is not something we like to think about, but with the world becoming increasingly more connected with each passing year, it is not a matter of if, but when, the world will be hit with the next global pandemic. It is critical we use the time between pandemics to help our health systems bolster existing monitoring solutions and workflows and activate a plan that can be drastically scaled. COVID-19 will undoubtedly transform how we prepare for and act during biothreats – today’s impromptu patient monitoring realities will push us from a reactionary approach, to pulling the necessary pieces in place when the clock isn’t ticking.

Share on social media
Topics
Author

Peter Ziese
Business Leader, Monitoring and Analytics, Philips Dr. Peter Ziese began his clinical career in 1990 at the University Hospital of Tuebingen in Germany, specializing in anesthesiology, with an interest in pediatric and cardiothoracic cases. He further specialized in intensive care and emergency medicine. In 1997, he joined Hewlett Packard as a clinical consultant and in the following years, took over responsibilities in telemedicine and key account management within the German healthcare organization of Hewlett Packard and Agilent Technologies. He joined Philips in 2001, working in international management and heading up first the marketing organization for patient monitoring and later on the sales and marketing center for Patient Monitoring and Critical Care Systems for Europe, the Middle East and Africa. Dr. Ziese has held numerous leadership positions and today, serves as Business Leader and General Manager for Monitoring & Analytics.
Follow me on