Five years from now, when we look back on how millions of healthcare professionals rose to the occasion to combat COVID-19 with unwavering commitment and pioneering use of the latest technology, will we see today’s crisis as a turning point for digital transformation in healthcare? It is my firm hope and belief that we will. Digital transformation has been on the agenda of healthcare providers for years – yet despite huge progress across the industry, fully rethinking healthcare for the digital age often remained an elusive long-term goal. Until the pandemic struck. COVID-19 has become a catalyst for change – a defining moment for all of us to reimagine healthcare the way it should be. That starts at the very beginning of the patient pathway, with precision diagnosis – the compass for effective treatment. Before the pandemic, diagnostic services were already burdened with high demand, short staffing, and inefficient workflows, leading to alarming rates of staff burnout. In the face of COVID-19, the need for greater efficiency and responsiveness has become even more urgent. And that need will only grow stronger. After an estimated 50-70% decrease in imaging volume during the peak of the pandemic, radiology departments will be tested to the limit as healthcare facilities resume elective exams and procedures for patients with cancer, heart disease, and other conditions, while continuing to support critical care for COVID-19 patients. Effectively juggling these responsibilities will require a new model of digital care delivery – founded on precise diagnostics and robust telehealth networks, organized end-to-end around patient pathways, centrally coordinated based on real-time analytics, and with workflows that adapt dynamically to rapidly changing circumstances.
COVID-19 has become a catalyst for change – a defining moment for all of us to reimagine healthcare the way it should be.
What does this mean for patients, diagnostic service providers, and healthcare IT leaders? Here are seven examples of how digital transformation in healthcare is shifting into a higher gear in response to COVID-19 – and how I foresee these developments continuing into the future.
1. Digital engagement helps keep patients safe and personalizes care
With severe disruptions of care delivery and increased anxiety among patients, effective communications between care providers and patients has never been more important – and challenging. Care providers such as the Boston Medical Center (BMC) have successfully used remote patient engagement to communicate quickly at scale with patients whose care plans have been impacted, while keeping their staff and patients safe. In the initial turmoil of COVID-19, BMC used personalized, automated text messages, emails, and voice calls in four languages to deliver targeted and precisely timed educational and instructional messages to over 400,000 BMC patients via the Philips Medumo platform. These messages ranged from tips to avoid the spread of COVID-19, to instructions on how to receive prescription refills through the mail. BMC also adapted its existing pre-visit education program to transition patients from in-person visits to telehealth consults, sending out reminders to help patients show up on time and prepared for their virtual appointments. As imaging services start rescheduling elective procedures, timely education and instructions will remain essential – with studies showing that automated reminders can lead to a 42% reduction in patient no-shows and a 67% reduction in poor patient preparation.
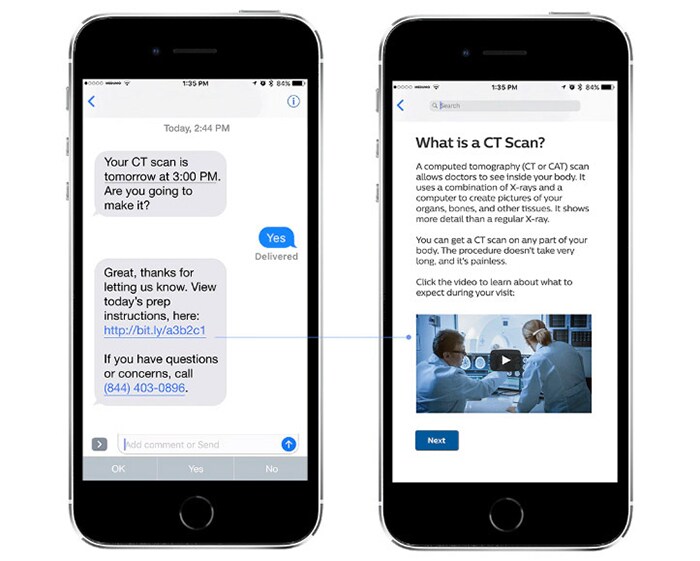
For patients, receiving timely messages on their smartphones also brings the convenience they have come to expect in today’s digital world. Spurred by COVID-19 and the need for physical distancing, a “waitless” waiting room for radiology exams is likely to become the new norm – providing up-to-the-minute text or voice scheduling updates to minimize lobby wait times, limit the chance of virus transmission, and allow patients to carry on with their busy lives right until the moment of their scan.
2. Portable ultrasound brings diagnostics to the point of care
Close to the front lines of care, the fight against COVID-19 has seen important roles for imaging modalities ranging from X-ray to CT – particularly in places where lab tests were scarce or turnaround times too long. But perhaps most strikingly, the crisis has highlighted the value of portable ultrasound in bringing diagnostics to the point of care: in the emergency department, intensive care unit (ICU), or makeshift triage tents. When COVID-19 first struck in the Chinese city of Wuhan, physicians turned to handheld ultrasound systems to assess patients for severe acute pneumonia, the life-threatening illness associated with the most severe cases of COVID-19. In Italy, doctors followed suit as they were desperately looking for ways to quickly assess patients in danger of respiratory failure. In response to those rapidly emerging needs, Philips recently received an industry-first FDA clearance for the use of our ultrasound portfolio – including Lumify handheld ultrasound – to manage COVID-19-related lung and cardiac complications.

By imaging COVID-19 patients at the point of care, physicians can perform diagnosis on patients and monitor progression of associated conditions without the need to move patients around the hospital, helping to reduce the risk of virus transmission. Images can be automatically transferred to the electronic medical record, accompanying patients throughout their care journey. I expect further uptake of portable ultrasound during and beyond COVID-19, as basic diagnostic capabilities move into new sites of care closer to the patient. At the same time, we also continue to see increased demand for X-ray and CT scans, with healthcare providers using the full gamut of imaging to diagnose suspected COVID-19 patients, and to monitor disease progression throughout the patient pathway.
3. Standardized presets and protocols help perform diagnosis first-time-right
Because healthcare professionals face a previously unseen threat in COVID-19, making the right diagnostic equipment available in the right place is only part of the solution. Equally important is that the equipment is quick and easy to use, even for less experienced users, to help them get consistent results under highly stressful circumstances. For example, in an effort to support radiology staff with fast acquisition of CT scans, we developed CT chest protocols for suspected COVID-19 patients. With staff sometimes reduced to one technician to reduce risk of exposure to COVID-19, having a clear and easy-to-follow protocol at hand helps to promote consistent image quality for first-time-right diagnosis or reliable disease tracking over time. Similarly, our Lumify portable ultrasound system comes with tissue-specific presets that support the examination of specific organs such as the lungs or the heart – allowing clinicians to quickly obtain relevant images at the point of care. In the same spirit, we are working with clinical partners around the world to adapt and expedite protocols in MR, now that imaging centers are facing a hefty backlog of elective exams. For example, by incorporating an acceleration technique that shortens MR exams by up to 50%, radiology departments can scan more patients and alleviate some of the burden on staff who must deal with new, COVID-related standards of care and disinfection.

4. Remote image reading surges – and enables real-time virtual collaboration
One massive change brought about by COVID-19 is that many radiologists, cardiologists, and oncologists were suddenly forced to work from home – creating an unprecedented need for home PACS workstations and secure clinical informatics solutions that allow them to read images remotely. For the department of radiology at the University of Alabama in the U.S. city of Birmingham, that meant completely redesigning their workflows. They rapidly deployed more than two dozen remote PACS workstations. Here’s how they did it. Interestingly, one recent survey among radiologists indicated that more than half of them saw enough benefit in their current workflows to consider continuing them post-COVID-19, with 65% reporting decreased stress levels. It’s a clear sign that remote reading could be a lasting change. As one of the early pioneers in digital transformation in pathology, we see a similar surge in remote reviewing of pathological cases, with the support of regulatory agencies who adapted regulation in the wake of the pandemic. Pre-COVID-19, pathology labs that digitized their workflows across different sites already reported improved collaboration and productivity gains of up to 21%.

The ability to share images instantly also creates new forms of collaboration. For example, using a tele-ultrasound platform, clinicians at the point of care are able to share ultrasound images and consult with a remote healthcare professional in a safe and secure way – all in real time. With a further shift to distributed diagnostics, there’s no turning back now. Virtual collaboration is here to stay.
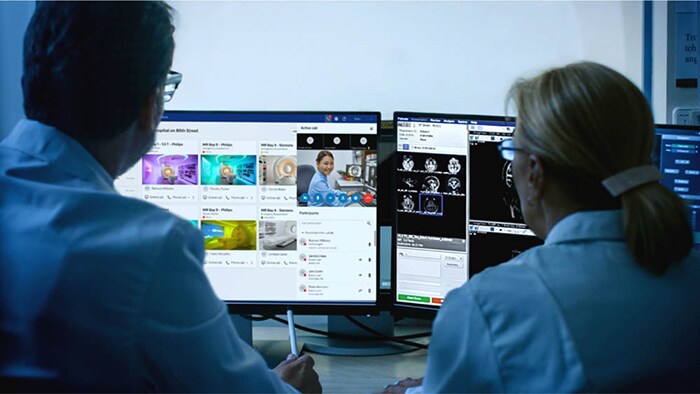
5. Central coordination is critical in adapting to demand and capacity changes
As distributed ways of working take hold, central coordination will be the linchpin for dynamic adaptation to changes in demand, capacity, and clinical conditions across sites, both inpatient and outpatient. In recent years, centralized command centers already started gaining traction in healthcare. These centers integrate data from various sites to steer clinical and operational decision-making in real time – much like other industries manage dynamic and complex operations in one place. Think of air traffic control towers that monitor and guide thousands of flight paths simultaneously, or smart cities that analyze traffic data in real time to optimize traffic flows and prevent congestion in busy areas. In healthcare, the need for central coordination has become even more pronounced because of COVID-19. During the crisis, we have seen clinical and operational management teams emerge that work closely together to respond to uncertainties in a highly agile way. These ad-hoc teams will evolve into established (virtual) command centers to coordinate diagnostic services. Staff will remain distributed across sites. But all relevant data will be in one place, to help enable real-time analytics and decision making.
6. Interoperability and patient data exchange are more vital than ever
When it comes to data sharing, COVID-19 has challenged healthcare providers in another way, too. Overwhelmed by the rapid outbreak of the virus, limited ICU capacity prompted hospitals in many countries to transfer patients to hospitals beyond their networks. This created an immediate need for seamless, secure sharing of medical information, while safeguarding patient privacy. In March, Philips collaborated with the Dutch government and two leading hospitals to create an online portal that connected 95% of all Dutch hospitals for digital exchange of COVID-19 patient data. We also continue to support healthcare IT leaders in other countries to build the necessary digital bridges, making it easier for overburdened networks to transfer patients to less impacted networks. It’s vital that we learn from this crisis in order to advance an agenda of greater interoperability and increased sharing of patient data, while protecting patient privacy. As one younger healthcare professional observed in this year’s Philips Future Health Index research, “being able to access records in an organized fashion from the comfort of my computer terminal seems like a no-brainer.” Except, it isn’t. Almost two thirds of younger healthcare professionals said that sharing restrictions often result in incomplete digital patient data. They cited improved interoperability between platforms as one of the top opportunities to ensure that digital patient data is used to its fullest potential. I couldn’t agree more.

7. Artificial intelligence helps turn data into fast and meaningful insights
Having all relevant patient data at hand goes a long way toward precision diagnosis that guides the right treatment decisions at the right time – but data without intelligence can leave healthcare professionals even more overwhelmed. In an effort to aid the rapid diagnosis of COVID-19, researchers around the globe are putting artificial intelligence (AI) to the test. In China, Philips partnered with Shukun Technology to jointly deploy an AI algorithm that can quickly characterize affected regions in the lungs based on chest CT, translating a scan into a report within 30 to 120 seconds to support the radiologist. Used by more than 20 hospitals in China in over 20,000 patient cases, the AI algorithm can also help analyze patient scans over time, enabling physicians to monitor disease progression in order to decide on patient discharge after successful treatment.

The value of AI in precision diagnosis goes beyond image analysis, however. In my view, AI is really about empowering the radiologist, the technologist, and the physician at every moment in the diagnostic journey. In the near term, I especially see opportunity for AI to speed up planning, scanning, and processing of exams. This will be critical in clearing the backlog of elective procedures, reducing waiting times for patients who are anxious to get their imaging exams rescheduled.
A defining moment to reimagine healthcare
Of course, achieving precision diagnosis is but one milestone in a patient’s journey through the healthcare system. My colleagues at Philips have detailed how COVID-19 is also accelerating innovation in image-guided therapy and connected care, introducing new ways to support caregivers and patients from the hospital to the home, across the health continuum, all building on interoperable digital platforms. It goes to show how the pandemic has been a lightning bolt for digital transformation in healthcare, bringing healthcare professionals, scientists, and IT experts together to turn necessity into invention. The future of digital healthcare is now. Let’s shape it together, with people at its center.

Share on social media
Topics
Author

Kees Wesdorp
Former Chief Business Leader Precision Diagnosis Kees Wesdorp led Philips’ Precision Diagnosis business cluster from 2020 to the end of 2022.













