As demand for medical imaging has grown dramatically over the last few decades, radiology workflow has become increasingly complex. With the ongoing COVID-19 pandemic adding to the pressure, radiology departments are embracing new and innovative ways of working that help them improve operational efficiency, patient and staff experience, and ultimately outcomes. Arguably the biggest challenge to optimizing radiology workflow is that it’s actually a complex web of separate workflows. Whether it’s getting a patient to show up on time for an imaging exam, acquiring the actual images, or getting the right clinical information in the hands of the referring physician, every step of the imaging process is susceptible to delays, variability, and gaps in communication – all of which cause waste and can have a negative downstream impact on patient care.
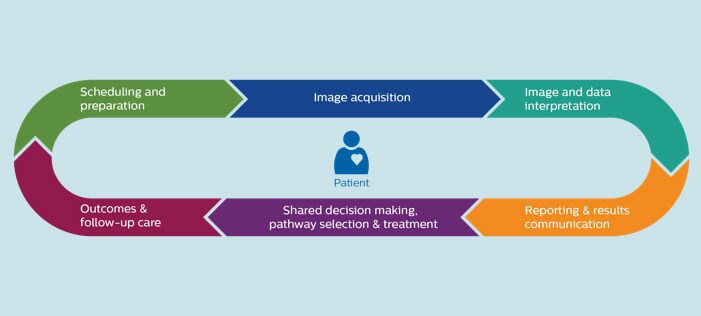
Managing such a complex and dynamic system can be a daunting task. It requires a clear view of the bigger picture, as well as a deep understanding of the daily challenges of all the individual stakeholders involved. Operational inefficiencies and disconnects weigh heavily on physicians and staff, who want the very best for patients but often find themselves scrambling for information and wasting precious time. COVID-19 has certainly not made things any easier. For certain imaging procedures such as MR and mammography, which declined up to 74-93% in the wake of the pandemic [1], some imaging centers now face significant patient backlogs, while face-to-face contact is still restricted and safety concerns add to staff stress and patient anxiety. But if there’s a silver lining, it’s how radiology services have adapted by finding new ways of connecting people, data, and technology. Let me share seven examples that show how digitization, virtualization, and integration can help create one seamless radiology workflow centered around the patient, for improved efficiency and quality of care.
1. Digital engagement keeps patient safe and helps prevent no-shows
Missed patient appointments are a constant challenge for radiology departments, with no-show rates as high as 7% for some modalities [2]. Patient no-shows disrupt workflow, leave staff and equipment underutilized, and may cost an imaging center financial losses of up to $1 million [3]. Patients themselves may suffer the consequences too, as delays in diagnosis and treatment can lead to irrevocable harm. It’s a problem that has taken on increased urgency in the wake of COVID-19, with hospitals looking for ways to ease patients’ anxiety and safely bring them back in for their radiology appointments. For Boston Medical Center (BMC) and Yale New Haven Health (YNHH), digitally engaging patients before and after their appointments is helping to involve patients in their care. Personalized text messages remind patients of their upcoming exams and make them feel at ease by sharing links to safety protocols and other helpful information. Patients also go through a digital COVID-19 screening, allowing staff to identify which patients are healthy and willing to receive care while minimizing risk for staff and patients alike. Once patients arrive for their appointment, they can check in via text. No longer do they need to physically congregate in a waiting room – they can now wait in the comfort of their car. Staff are alerted via the Electronic Health Record system that the patient has checked in. Once they are ready to see the patient, a new text message is sent to the patient, inviting them in. Creating a virtual waiting room with contactless check-in has already saved front-line staff at BMC and YNHH a combined 4,918 phone calls to patients [i], and provides reassurance to patients who may otherwise be hesitant to come in.
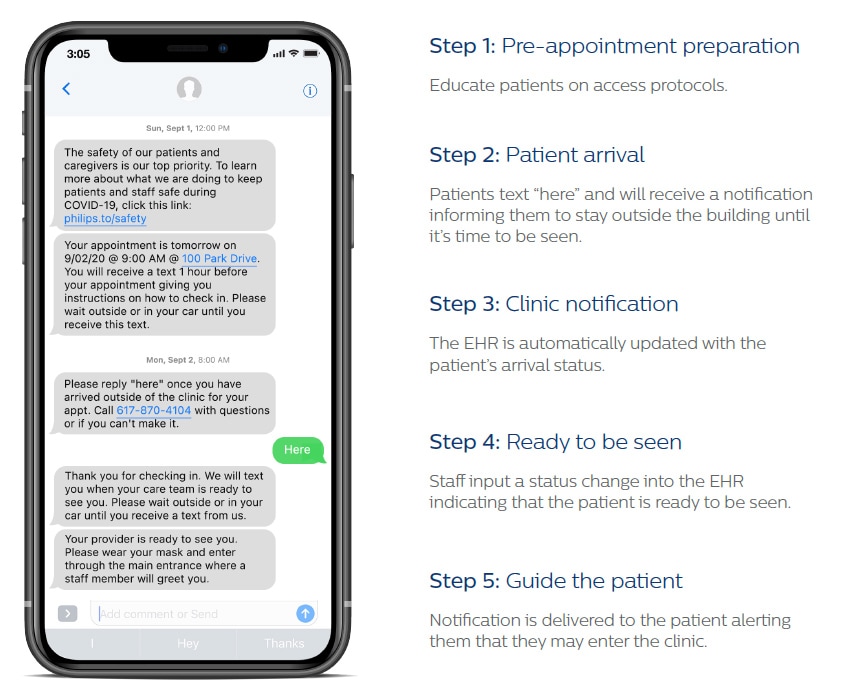
The virtual waiting room in action: patients check in contactless via text messages Text-based communications is also a powerful tool for helping patients and staff prepare for imaging exams. For example, using the same digital patient management platform, patients undergoing a CT scan may receive instructions about what not to eat and drink prior to the exam. They can also be screened for allergic reactions to contrast dye, alerting the care team to the possible need for pre-medication. Similarly, patients scheduled for an MR exam may be asked whether they have any metal implants, helping staff prepare the right protocol for optimal image quality. It shows how digital engagement can not only lower the barrier for patients to come into the hospital – it can also set staff up for success in the next phase of the process: the acquisition of the images.
2. Workflow automation assists staff in getting images first-time right
Radiology technologists have the daily challenge of achieving best-quality, first-time-right scans. But variabilities in the training and experience levels of individual staff can impact outcomes. Patients are often anxious, too, which increases the pressure on technologists to get the exam done effectively because a restless patient can mean redoing the exam. Yet staff often have little time to interact with patients, because their workload can be relentless [4]. When we surveyed radiology technologists what would help them most, they said 23% of their work is inefficient and could be automated. Taking those needs to heart, we have developed smart workflow tools that help technologists perform exams with more ease and less stress. For example, in MR – arguably the most stress-inducing imaging modality – technologist workload can be reduced by automating exam planning, scanning, and processing. This allows even new technologists to perform routine MR exams with confidence. Decreased exam variability results in high-quality imaging that supports confident diagnosis, while automated patient coaching enhances patient experience. Staff have to worry less about getting equipment settings right and have more time to focus on the patient.

Of course, for the most complex MR procedures, guidance from a more experienced expert in acquiring the images may still be needed. But what if that expert is not around or available? That’s when a different kind of support may be needed.
3. Image acquisition goes virtual with a central command center
Highly experienced technologists who know the ins and outs of advanced modalities such as MR and CT are often in short supply within large imaging practices that have multiple scanning locations. Until recently, these expert users would have to travel from their central location to remote sites to help out their less experienced colleagues. But now they can provide assistance at multiple locations in real-time while the patient is on the scanner table – without having to leave their central location. Through a new form of tele-presence in image acquisition, expert technologists can provide guidance, support, and training from one central location: the Radiology Operations Command Center. Secure virtual scanner access enables these expert users to assist or train their colleagues across locations, thereby driving consistency in image quality and standardization. This reduces the need for unnecessary recalls and repeats, which can be a heavy burden on patients and on staff.

This cloud-based hub-and-spoke model can be easily scaled across several or even hundreds of sites. It makes imaging operations less vulnerable to local staff turnover, staff call-outs, and other unforeseen disruptions. In times of COVID-19, this has proven to be particularly valuable in ensuring business continuity, even when staffing was severely constrained at certain imaging sites. Having a central command center also allows imaging providers to offer complex procedures at more locations, closer to where patients live, and at more flexible hours. For patients, that means less hassle and more convenience, while having the peace of mind that a super-expert is looking over the technologist’s shoulder – even if it’s from hundreds or thousands of miles away. Once images are acquired, it’s important that the most urgent cases are delivered to the most qualified radiologist to expedite reading and reporting. That’s where another workflow innovation comes into play.
4. Intelligent workload balancing prioritizes the most urgent cases
In complex, multi-site radiology enterprises, where different locations generate an ongoing stream of imaging cases – some urgent, some less urgent, and some highly specialized – it can be a real challenge to manage the prioritization and delegation of cases to the best-suited radiologist. Intelligent algorithms that automatically determine the best match can help deliver the right case to the right radiologist, based on their area of expertise, availability, and current workload. This helps with workload balancing among radiologists, allowing the most urgent cases to be read first by the appropriate subspecialist who is available.

Intelligent algorithms can automatically assign and prioritize cases for reading by the best-qualified radiologists (patient names in this screenshot are fictitious) For example, when a patient with a sudden and acute headache is rushed into the emergency department and a CT scan reveals bleeding inside the brain, that scan will automatically appear on top of the worklist of the neuroradiologist who is available at that moment. While the patient is still in the scanner, the radiologist reading the image can remotely connect to other specialists to discuss the case in a secure digital environment, giving the patient the best chance of timely diagnosis and effective treatment. This brings us to the next challenge in the radiology workflow: giving the referring or responsible physician the information they need, in a way that is easy to access and offers the right clinical insight.
5. Interactive multimedia reporting offers physicians deeper insight
Ever since Wilhelm Röntgen discovered the X-ray 125 years ago, radiology reports have not fundamentally changed in format – relying on a text-based narrative to convey findings to physicians and patients [5]. But that is now changing, with radiology reporting moving into the multimedia world that already surrounds us in our everyday lives. In oncology and other complex clinical domains, where patients are often followed over long periods of time, physicians are looking for rich and longitudinal insight in radiology reports, without having to dig for prior reports and manually compare images. Interactive multimedia reporting allows radiologists to embed key images for side-by-side comparison, tumor trending information in charts and graphs, and quantitative data from advanced post-processing.
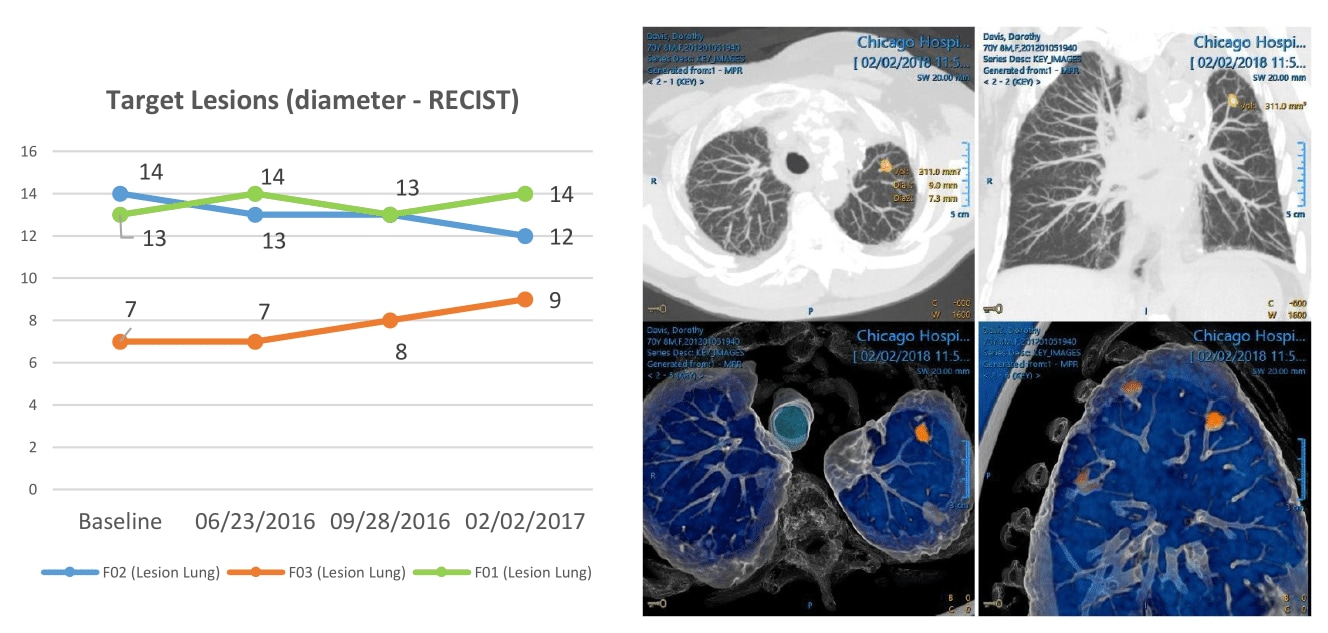
Interactive multimedia reports give physicians direct access to key images and relevant quantitative information Physicians can now click on the embedded images for closer inspection without having to leave the report. This can be a big time-saver. One study showed how multimedia reports can save oncologists 8.9 minutes in assessing a patient’s tumor burden compared to text-only reports [6]. Multimedia reports also enable further assessment of disease features beyond what is communicated in the text, for example in light of new clinical questions that are relevant to the patient’s treatment. By offering direct access to key images from the radiology report, we are streamlining the flow of information from radiologists to referring physicians – an approach we can take even one step further.
6. Integrating patient data supports clinical collaboration
In a domain as complex as cancer care, where imaging studies are complemented by many other types of information including pathology reports, molecular tests, and genetic profiles, it can require a huge effort to pull together all relevant patient information from disparate departments for treatment selection and monitoring. This is where care teams often lose precious time today. By creating unified dashboards that automatically integrate patient information from multiple departments, cancer care teams can see the whole patient profile at a glance and decide on a treatment pathway during multidisciplinary tumor board meetings. These meetings can be attended virtually or in-person, allowing for flexible and effective collaboration based on a shared overview of all relevant data.

Once the most appropriate care pathway has been decided on, it often requires further diagnostic studies to monitor disease progression and treatment effectiveness, which brings us full circle: how to ensure that patients show up for their follow-up exams.
7. Real-time, data-driven operations enable continuous improvement
We’ve already seen the value of digital engagement in educating patients and reminding them of their appointments. This, coupled with automated follow-up tracking, can be a great help in getting patients to follow through on their treatment plans. But what if you could identify, based on patient data, which patients are most likely not to show up for follow-up exams – and give them additional attention? Studies have shown how patient no-shows can be predicted based on previous no-shows, days between scheduling and appointments, and modality type – allowing radiology administrators to target their patient engagement efforts more precisely [7]. It’s just one example of how data-driven practices can help improve continuity of care and operational efficiency in imaging enterprises. Real-time data analytics has created other opportunities for operations management as well. By giving radiology administrators the tools to continuously monitor KPIs such as modality-specific exam volumes, resource utilization, and cancellation rates, they can also get a better understanding of how patient engagement is changing the demand for services. This allows them to make better informed decisions on allocation of staff and resources, based on the latest facts and figures.
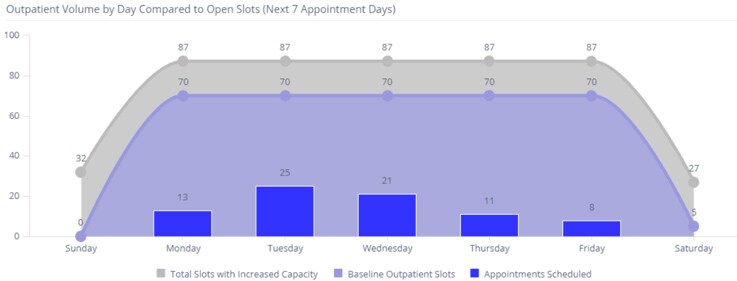
Real-time data analytics helps radiology administrators optimize staff and resource allocation For example, as radiologists departments are ramping up again in the wake of COVID-19, we are helping them create dashboards that forecast how many technologists are needed for particular shifts based on expected patient volumes. These dashboards also give a better grasp of how COVID-related safety and cleaning protocols are affecting throughput and capacity, allowing them to adapt scheduling where needed. Dashboards are updated on the fly – constantly helping administrators decide what to do next.
One integrated radiology workflow for precision diagnosis
What these seven innovations show is how digitization, virtualization, and integration – supported by real-time data analytics – can make a real difference to radiology operations. Especially now. By connecting data, technology, and people at every defining moment – always with the patient firmly at the center – we can pave a clear path to precision diagnosis and treatment. That’s when radiology workflow really flows – benefiting patients, staff, and the health systems that care about them both. Join us at RSNA 2020 from November 29 to December 5 and register for our virtual sessions to find out how radiology leaders from leading institutions are addressing their workflow challenges. References [1] Naidich J.J., Boltyenkov A., Wang J.J., Chusid J., Hughes D., Sanelli P.C. (2020). Impact of the Coronavirus Disease 2019 (COVID-19) Pandemic on Imaging Case Volumes. J Am Coll Radiol, 17(7):865-872. https://doi.org/10.1016/j.jacr.2020.05.004 [2] Rosenbaum J.I., Mieloszyk R.J., Hall C.S., Hippe D.S., Gunn M.L., Bhargava, P. (2018). Understanding Why Patients No-Show: Observations of 2.9 Million Outpatient Imaging Visits Over 16 Years. J Am Coll Radiol, 15(7):944-950. https://doi.org/10.1016/j.jacr.2018.03.053 [3] Rebecca J., Mieloszyk, J.I., Rosenbaum, C.S., Hall, U., Puneet B. (2018). The Financial Burden of Missed Appointments: Uncaptured Revenue Due to Outpatient No-Shows in Radiology. Current Problems in Diagnostic Radiology, 47(5): 285-286. https://doi.org/10.1067/j.cpradiol.2018.06.001 [4] Beker, K., Garces-Descovich, A., Mangosing, J., et al. (2017). Optimizing MRI Logistics: Prospective Analysis of Performance, Efficiency, and Patient Throughput. American Journal of Roentgenology, 209(4): 836-844. https://doi.org/10.2214/AJR.16.17698 [5] Folio, L.R., Machado, L.B., Dwyer, A. (2018). Multimedia-enhanced Radiology Reports: Concept, Components, and Challenges. RadioGraphics, 38(2): https://doi.org/10.1148/rg.2017170047 [6] Folio, L.R., Yazdi, A.A., Merchant, M., Jones, E.C. (2015). Initial Experience with Multi-Media and Quantitative Tumor Reporting Appears to Improve Oncologist Efficiency in Assessing Tumor Burden. Research findings presented at the 101th Scientific Assembly and Annual Meeting. http://archive.rsna.org/2015/15005140.html [7] Harvey, H.B., Liu, C., Ai, J., et al. (2017). Predicting No-Shows in Radiology Using Regression Modeling of Data Available in the Electronic Medical Record. J Am Coll Radiol, 14(10):1303-1309. https://doi.org/10.1016/j.jacr.2017.05.007 Notes [i] Internal data results are specific to the institutions where they are obtained and may not reflect the results achievable at other institutions.
Share on social media
Topics
Author

Kees Wesdorp
Former Chief Business Leader Precision Diagnosis Kees Wesdorp led Philips’ Precision Diagnosis business cluster from 2020 to the end of 2022.













