Soon after COVID-19 cases first spiked, something eerie happened – other patients vanished. Spooked by risks still largely not understood, patients dealt with their healthcare like they dealt with the virus, that is, by staying home. We saw this firsthand with our radiology partners: appointments were cancelled en masse. Anecdotally, some institutions reported a greater than 70% drop in imaging volume in the outpatient setting and around 50% drop in the inpatient setting [1]. A backlog of appointments quickly piled up, and they needed to be rescheduled. Yet patients were confused about how to do so and if it was even safe. Health systems struggled to engage these patients – let alone convince them that safety protocols were in place. They urgently needed a plan to resolve the backlog, quickly and safely. The answer, it turns out, was right on our phones. Within weeks of hearing from our customer-partners about this problem, we launched new digital outreach programs through Philips Patient Management Solution. Since then, we’ve been helping these healthcare leaders re-engage patients, reduce backlogs, bring patients back into radiology departments, and connect them to virtual visits. These new, innovative approaches are still in development, but the early results are promising. These programs enable a better, more diverse way to deliver care, and I believe they are a glimpse into the future of diagnosing, managing and treating patients virtually. At the most fundamental level, the pandemic has highlighted the need for health systems to implement a scalable digital strategy to reach patients directly. So as new challenges emerged during the pandemic – mass cancellations, rebooking, navigating the return to operations, bringing a backlog of patients back into the fold – we’ve worked with our partners to build digital strategies capable of addressing them head on. We’ve found three things that have been key to overcoming these challenges:
1. New forms of patient navigation are urgently needed
With the virtual waiting room, health systems can continue their operations while following safety protocols. Patients check-in from their phones via text when they arrive at their appointment, then remain in their car, entering the hospital only after they get a new message that the staff is ready for them. On the staff side, the care team is alerted in the electronic medical record (EMR) that a patient has checked in; then the care team indicates in the EMR that they are ready for the patient, and a new message is sent to the patient instructing them to come inside for their visit. Yale New Haven Hospital and Boston Medical Center, where we first launched virtual waiting rooms in mid-August, have been instrumental partners in developing this technology. Combined data from these two heath systems show that, since offering virtual waiting rooms, patients have spent 877 fewer hours in physical waiting rooms. Moreover, front-line staff have made 4,918 fewer calls to patients because our contactless check-in process has removed the need for staff to make manual phone calls to these patients.[i]
Before our partners could resolve their backlogs, they had to figure out a way to deliver care during the pandemic. Just as many facets of our lives became contactless, we developed a ‘virtual waiting room’ that uses a text messaging check-in system to minimize the number of people sitting in a waiting room prior to their appointments.
2. Digital patient management unlocks virtual care, can help resolve backlogs
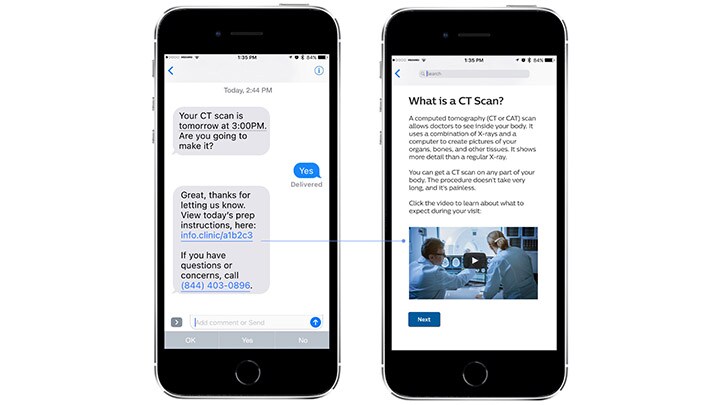
Since the pandemic hit, Philips has rapidly expanded our message broadcast capabilities. This has given our customer-partners the ability to inform their patients of new infection control protocols, changes to hours of operations, and public health announcements. We’ve also enhanced our automated appointment navigation programs to help bring patients back into the fold after their appointments were canceled, adding in COVID-19 screenings and information about pre-visit testing. Because many patients don’t feel comfortable coming in for radiology appointments, this style of messaging also helps assess patients’ unease and provides education to explain how safety protocols have been adapted in response to COVID-19.
3. New tactics address socioeconomic barriers to patient management
As COVID-19 impacted Boston, hotspots flared in lower socioeconomic and non-English-speaking communities. Not every patient has access to digital technology, and, unfortunately, patients with the least access often need the most care. Our local partners wanted to create programs to help those populations. That’s why we developed a multi-channeled approach, so that patient outreach could be conducted with or without internet access. We created a COVID-19 education program in patients’ native languages – seven in total, including Spanish, Portuguese, and Haitian Creole – and delivered it using text messaging. We used this approach to deliver COVID-19 education for staff as well. Thus far, we’ve sent 670,000 messages to over 70,000 patients and staff in the greater Boston area. [i]
Building a new standard of care via digital patient management
COVID-19 has been a forcing function for all of us to accelerate what I believe will be the healthcare experience of the future. It has increased patient and physician openness to new ways of interacting – and it has streamlined new workflows related to virtual care encounters. There is still much work to do to realize the full potential of digital patient management – we must go beyond focusing on encounter-based care and move into the realm of population health and chronic care management. This will allow us to achieve a more holistic and cohesive patient experience, stitching together the diverse venues where care is provided and strengthening the patient-physician relationship. I firmly believe that engaging with patients in this way will become the new standard of care, because it creates nimbler health systems, lowers the cost of care, increases access and provides more patient-centered touchpoints, which all drive toward value-based care. It is undoubtedly a better way to serve our patients. [i] Internal Data Results are specific to the institutions where they are obtained and may not reflect the results achievable at other institutions. References: 1 Cavallo JJ, Forman HP. The Economic Impact of the COVID-19 Pandemic on Radiology Practices [published online ahead of print, 2020 Apr 15]. Radiology. 2020;201495. doi:10.1148/radiol.2020201495

Share on social media
Topics
Author

Adeel Yang, M.D.
Clinical Leader, Patient Management at Philips Prior to joining Philips, Yang was co-founder and CEO of Medumo, a Boston-based digital health company providing patient management and software services to healthcare providers. He completed his M.D. at the University of Arizona with research distinction and holds multiple patents and publications.
Follow me on













