How a global pandemic changed one hospital’s approach to transitional respiratory care: A Q&A with Dr. Javier Sayas Catalán
As the COVID-19 pandemic began to spread across the globe, physicians and specialists quickly convened – face to face and even remotely across oceans – to better understand their options and resources for treating those infected with this new and aggressive respiratory disease. Treatment options varied greatly depending on levels of patient severity, but one challenge was clear and consistent: the growing need for critical care ventilators. Philips offers industry-leading respiratory solutions including invasive and noninvasive ventilation (NIV), oxygen therapy, positive airway pressure (PAP) therapy, nebulizers, airway clearance, patient monitoring software, and medical consumables that can help health systems and clinicians as they navigate this complex and dynamic environment. For nearly 40 years as a pioneer in the field of respiratory innovation, Philips has collaborated closely with health systems, clinicians, homecare providers, educators and government officials to support a patient-centered and coordinated respiratory disease management approach. Dr. Javier Sayas Catalán, a pulmonologist at Hospital U 12 de Octubre in Madrid, Spain specializing in non-invasive ventilation therapy, has been collaborating with Philips in this capacity for many years. He and his teams seek and receive critical guidance while providing real-world feedback on Philips polysomnography and ventilation solutions, which allows for continuous improvement and an enhanced ability for Philips to meet customer and patient needs through cooperative innovation. So when the pandemic reached his 1,300 bed hospital in Madrid, he felt he had a solid footing when it came to finding creative, yet safe and effective ways to treat the new wave of patients presenting with respiratory insufficiency. In this interview, Dr. Javier Sayas Catalán shares his experience in treating these patients using Philips Trilogy Evo, and how it’s changed the way he and his team administer respiratory care. Q: What is a normal day like with you and your team? JSC: Our hospital offers complete pulmonary service as well as NIV neuromuscular clinic and respiratory intermittent care. We specialize in anything related to NIV, both acute care and in the homecare setting. We work with many patients from our lung transplant program who suffer from COPD or Cystic Fibrosis. There are three physicians in my NIV unit and we work very closely with our colleagues in the ICU. Our homecare practice is divided between intermediate care and inpatient care in the regular ward and outpatient care and we make a point to keep track of the ongoing progress of every patient we start on NIV therapy. For example, a COPD patient that may need to start acute NIV, we help them to get set up. If they need chronic home NIV, we will support that transition and follow-up in outpatient care. Our team’s strength is that we take care of every single patient throughout their entire journey, from acute care all the way through continuing homecare therapy. It’s important to follow along in the patient’s journey closely to ensure they are receiving the highest level of care. So equipment and technology that better enables us to do that is always in high demand. Q: When did you first begin to introduce Philips solutions in to your practice? JSC: We have worked with Philips polysomnography equipment for a very long time, so I’ve always been familiar with the level of clinical expertise they offer with their solutions. For the past 5-7 years, I’ve been using Philips ventilation equipment as well. Lately, I’ve been more involved with testing and providing feedback for these solutions. Philips representatives listen to and truly hear demands about how devices work and perform, how they could be improved, and how clinicians use – or need to use – them in a real world setting. It’s a true give-and-take relationship. It’s nice to have someone on the manufacturer’s side who is willing to listen and improve their solutions based on feedback. Increasing cooperation is a key to a solid working relationship.
If you are adapting a patient to chronic NIV in the hospital, it’s helpful to assure that there is continuity on the ventilator that they will eventually be using at home.
Dr. Javier Sayas Catalán
Q: How has this pandemic changed the way you administer care? JSC: The vast majority of COVID-19 patients experienced hypoxic respiratory failure. In some cases early on, we used CPAP treatment for the less severe patient cases and saw an increased demand for CPAPs in the hospital setting on a broad scale. We used what we had. The more severe patients, however required invasive mechanical ventilation in the ICU. Trilogy Evo with OBM allowed us to shift not only in the most acute phase, but for patients who were weaning coming from the ICU to our intermediate care unit. As the demand for very high-tech, hospital-grade ventilators increased, we set patients on Trilogy Evo who perhaps didn’t require all of the bells and whistles of a dedicated ICU ventilator or Philips V60 ventilator, for example... We used those vents to free up ICU vents for more severe patients. Having access to Trilogy Evo with OBM allowed us to increase our ventilation treatment significantly during the pandemic. The hospital now has six more Trilogy Evo ventilators on top of what we had previously. In my opinion, Trilogy Evo will become one of the key ventilators for our respiratory care service. Trilogy Evo is versatile enough that it allows for use across multiple care settings and easy transitions. It’s very user-friendly as kind of a “mini V60” with simplicity in setting pressure and frequency, setting up patients or changing modes, but as powerful as a V60. On the one hand we can keep the art of ventilation with fine-tuned settings, and on the other hand we have an easy-to-use solution that allows us to ventilate acute patients without overcomplicating the treatment process. Q: What led you and your colleagues to choose Trilogy Evo as a care solution? JSC: We had known about Philips Trilogy ventilators for some time. We had tested Trilogy 100 in many different patient scenarios, so we were familiar with the reliability of the Trilogy line of ventilators. Many months before the pandemic was even a whisper, we were able to test Trilogy Evo and noticed that it maintained the strong aspects of the original Trilogy, but added flexibility in terms of circuits, O2 inputs, improved pressurizations, and the ability to deal with higher FiO2. Another important feature is that pressurization rate has improved quite significantly in the Trilogy Evo, when compared with the Trilogy 100, as well as turbine performance. It can support very rigorous environments – moving from EU, to intermediate care or to ICU – and is very easy for non-trained personnel to quickly grasp and operate efficiently with ease. The main advantage it presented was the flexibility. We could use it in an acute care setting thanks to the improved pressurization and ability to accept an O2 blender. When we began to think about how to prepare for the COVID-19 crisis, we thought immediately about using Trilogy 202 with an added oxygen port, as Trilogy 100 may not accept very high oxygen input flows. When Philips presented Trilogy Evo with oxygen blender module (OBM), it was a very straightforward decision. We bought six Trilogy Evo ventilators, allowing us to treat many very sick patients. Q: You mentioned transitions in care settings, can you explain further how this impacts treatment? JSC: The great thing about Trilogy Evo is that we can keep patients on the same track from an acute through a post-acute setting. It allows us to discharge patients with the same technology that is used to treat them in the ICU. If you are adapting a patient to chronic NIV in the hospital, it’s helpful to assure that there is continuity on the ventilator that they will eventually be using at home – the same settings, triggering, data, etc. It may not be the same physical box, but they will have an understanding and familiarity with the equipment and how we used it to treat them and we will have a comparable view of their progress. Also, similar technology means similar turbine behavior, keeping the same performance and adapting to patient’s demands. So, if the homecare provider has the ability and inventory to help send a patient home with the same device we used to treat them in the hospital, it is ideal. Q: How have you witnessed ventilation technology evolve over the past few years? JSC: There has been a huge improvement with the way ventilation technology works. Previously, we did not use these types of ventilators for acute COPD patients, choosing other equipment due to some lack of performance when the patient exhibits high inspiratory demand. Rather, we used them predominantly for neuromuscular patients. The equipment and technology have drastically improved by way of versatility. For example, Trilogy Evo has improved pressurization capabilities and we are now able to use it for exacerbated COPD patients better than we ever had before. Monitoring capabilities, both remote and on-site, are the other game-changing features, allowing for a high degree of controlling and tailoring ventilation parameters. Q: What advice or guidance would you offer to colleagues or other industry professionals experiencing this new normal worldwide? JSC: Be open-minded. Many of my ICU colleagues are quite strict about using only dedicated ICU vents for each and every patient, but they might find that the use of NIV or home ventilators in this type of environment can help to free up ICU ventilators in low-demand patients. Being open minded enough to use a different type of equipment that still offers the safety and efficiency you need to treat your patient appropriately could help you to assign resources more efficiently in a time of great need. During the pandemic, we worked to help train other hospitals in Spain. We conducted webinars to help other Trilogy Evo users to better understand and get used to using the device with challenging patient cases. It is important to share learnings with one another about what works well and what can be improved or modified to meet patient and facility needs. With this complex and changing world, it is impossible to innovate alone. Finding better solutions and creating value requires collaboration between different types of people and very different types of organizations. Philips believes that, in order to transform the delivery of health and build a sustainable business in this challenging context, we need a different, more human centered approach to innovation. Philips relies on physicians like Dr. Javier Sayas Catalán to help us achieve our mission of improving lives through meaningful innovation that is deeply rooted in clinical science. Real world feedback is what helps Philips to better understand and innovate solutions that provide integral care that not only improves, but can also save lives.

Share on social media
Topics
Contact

Meredith Amoroso
Philips Global Press Office Tel: +1 724-584-8991
You are about to visit a Philips global content page
Continue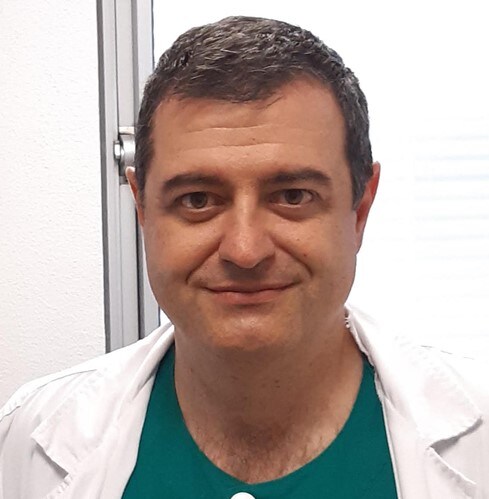
Dr. Javier Sayas Catalán, pulmonologist at Hospital U 12 de Octubre in Madrid, Spain