Bert van Meurs
Chief Business Leader, Image Guided Therapy, Philips
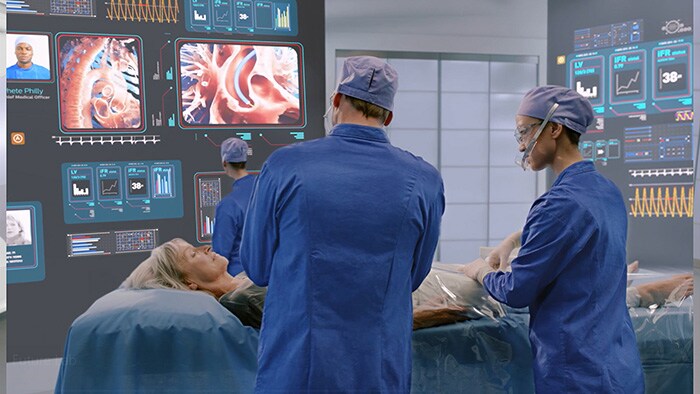
In metropolitan areas around the world, most hospitals today are equipped with state-of-the-art systems and devices that allow clinicians to perform image-guided minimally invasive procedures. Compared to traditional open surgery, these procedures provide significant benefits for patients, who typically recover faster and have a better treatment experience, and for healthcare providers, who can treat more people at a lower cost. But what about a patient in a remote rural area who is suddenly caught by a heart attack or stroke? The nearest big-city hospital may be many hours of travel away, severely decreasing the patient’s chances of timely treatment and survival. Much remains to be done to make image-guided therapy accessible to those who need it, regardless of where they live. Especially in a time when travel options have become even more limited for some of the most vulnerable patients due to COVID-19, we need to rethink where and how care is delivered. Not only to meet today’s challenges, but also to ensure that healthcare systems are fair and future-proof in the long run. Telehealth is part of the solution, but not a substitute for physical interventions.
Especially in a time when travel options have become even more limited for some of the most vulnerable patients due to COVID-19, we need to rethink where and how care is delivered.
How can we bring image-guided therapy closer to patients worldwide? Let me share some examples of first initiatives in that direction; most already underway before the pandemic, some further accelerating as a result of it.
Bringing image-guided therapy to rural areas in China
China is one country where large geographical divides in access to care still exist. Medical institutions and highly-qualified healthcare providers in China have historically concentrated in cities, leaving people in rural areas in a disadvantaged position because they have to travel for many hours to reach the nearest healthcare provider [1]. Fortunately, substantial progress is being made to close the gap between urban and rural healthcare services.

At Philips, we are working together with county-level hospitals in China to bring care closer to rural patients. One way we are doing this is by setting up local treatment centers for patients with chest pain or stroke. These centers take an integrated approach that covers the entire care pathway: from early diagnosis of a patient’s condition in the ambulance and further diagnostic tests in the hospital, to minimally invasive procedures in the cath lab and patient monitoring in the ICU. Supported by seamless data exchange across settings, this integrated approach helps to get patients to appropriate and effective treatment as soon as possible, followed by the right after-care.
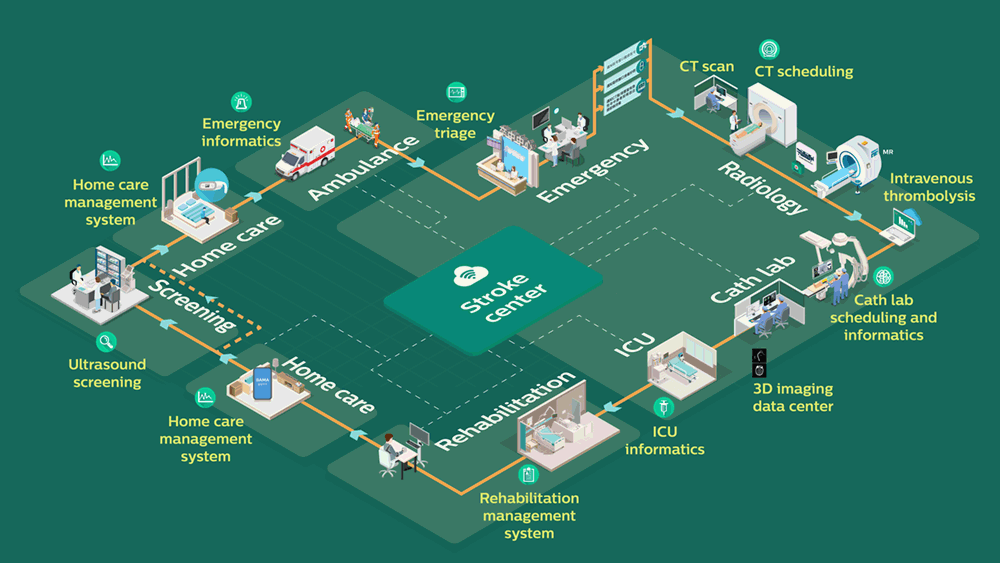
The Stroke Center in operation: one integrated patient pathway from diagnosis to minimally invasive treatment and aftercare, supported by seamless data exchange across settings
Setting up cardiology centers in India’s tier-two and tier-three cities
In India, another vast country where cardiovascular diseases are taking a growing toll, there is a similar expansion in the number of patients outside metropolitan areas that can now be treated with minimally invasive procedures. It’s a much-needed development. In the shadow of the rapid growth of India’s tier-one cities, patients in tier-two and tier-three cities have long had limited access to quality healthcare – a troubling fact for a country in which 1.7 million people die of heart disease each year [2]. New hope for previously underserved patients is now on the horizon. Following the launch of the government’s flagship health insurance program Ayushman Bharat in 2018, which makes healthcare more affordable for low-income families, major Indian hospitals are expanding their reach to tier-two and tier-three cities. As an example, we are partnering with Artemis Hospitals to set up hospital-based cardiology centers in multiple locations across the country. These centers will provide the much-needed access to high-quality care for populations that in the past had to travel long distances for such care. The aim is to offer an integrated solution for both emergency care and elective procedures, with a complete range of diagnostics, cath labs, and post-procedure ICU care that covers the entire patient pathway.

Together with Artemis Hospitals in India, we are setting up cardiology centers across the country to bring high-quality care closer to patients in tier-two and tier-three cities Although the dynamics are obviously different in each country, empowering locally based clinicians to perform minimally invasive procedures is a trend we see around the world. In countries where image-guided therapy is already more established, like the U.S., it has even begun to extend beyond the walls of the hospital – and with good reason.
Moving procedures to out-of-hospital settings in the U.S.
Today, image-guided therapy is typically conducted in a hospital. But as image-guided systems and devices become more advanced, certain procedures become more routine – which means they may not always require patients to come into the hospital. Instead, procedures can be carried out more quickly and less expensively in outpatient settings such as office-based labs (OBLs) or ambulatory surgery centers (ASCs), which offer a comfortable care environment that is more convenient for patients. Not only does the shift to these outpatient settings make care more accessible to patients – in a country like the U.S., it is an economic necessity. Driven by the aging of the population, the prevalence and costs of cardiovascular disease in the U.S. are expected to increase dramatically in the next 15 years, with total costs reaching $1.1 trillion by 2035 [3]. As the number of patients continues to grow, the current hospital-centric model of care will become financially unsustainable. Recognizing this reality, the U.S. Centers for Medicare & Medicaid Services (CMS) announced last year that low-risk percutaneous coronary interventions performed in ASCs will be reimbursed starting 2020. The impact could be significant. CMS estimated that moving 5% of coronary interventions from hospital settings to ASCs would reduce Medicare payments by about $20 million this year alone [4]. In the wake of COVID-19, I expect a further shift of interventional procedures to settings outside of the hospital. At the height of the pandemic, OBLs and ASCs helped relieve pressure from hospitals, offering an alternative for patients who would otherwise have suffered from a delay in care. Now that hospitals are still adapting to new, COVID-19-related standards of care, and patient backlogs remain, collaboration across care settings can help ensure that patients receive timely treatment.

In the U.S., a further shift of minimally invasive image-guided procedures to out-of-hospital settings is expected in the wake of the COVID-19 pandemic CMS seems to concur, with new proposed rulemaking announced in August. According to CMS, the COVID-19 pandemic has “highlighted the need for more healthcare access points throughout the country”. It is proposing to eliminate the list of services that can be done on an inpatient-only basis for Medicare patients over the next three years, which would create more flexibility for patients to choose ASCs and OBLs as a site of care. In the long run, partnering with OBLs and ASCs allows hospitals to expand their reach and lower cost of care, while providing a safe and convenient option for patients seeking care close to home – especially as additional procedures get approved for an OBL or ASC setting.

Raising community awareness for minimally invasive treatment
The benefits of ASCs and OBLs don’t end there. Increased presence of interventional specialists in local communities can also help raise awareness for the possibilities of minimally invasive procedures. Today, less well-known but debilitating diseases such as peripheral artery disease often go unrecognized, especially in poor rural areas. People don’t realize that having difficulty walking may be indicative of clogged arteries in their legs. The prospect of a long drive to a large and intimidating hospital can deter them as well. Tragically, they may only make the drive when it’s too late and their leg needs to be amputated. It’s an outcome that could have been prevented with early diagnosis and treatment. Having an outpatient lab nearby can make a big difference here – potentially saving people a limb. This does not mean that hospitals will become any less relevant in the delivery of image-guided therapy. Instead, I believe that both types of interventional settings complement each other. Shifting low-risk routine procedures to outpatient labs, where they can be performed more efficiently, frees up resources in hospitals to handle complex high-risk procedures. Ultimately, this means that more patients can be treated effectively and affordably. And that’s what should inspire us all as we continue to make image-guided therapy more widely available around the world. Because whether it’s a stroke patient in rural China, a heart patient in one of India’s smaller cities, or a vascular patient in an underserved community in the U.S.: every patient matters. References [1] https://www.sciencedirect.com/science/article/pii/S2352013214000726 [2] http://www.healthdata.org/india [3] http://www.heart.org/idc/groups/heart-public/@wcm/@adv/documents/downloadable/ucm_491543.pdf [4] https://www.tctmd.com/news/cms-finalizes-rule-allowing-reimbursement-pci-ambulatory-centers
Share on social media
Topics
Author

Bert van Meurs
Chief Business Leader of Image Guided Therapy, Chief Business Leader of Precision Diagnosis (ad interim) Bert van Meurs is Chief Business Leader of Image Guided Therapy, Chief Business Leader of Precision Diagnosis (ad interim), and is responsible for Diagnosis & Treatment. He is also a member of the Royal Philips Executive Committee.
Follow me on