The Future Health Index 2021 report is out and the results are striking. This year we polled healthcare leaders and uncovered some of the most surprising insights since the Future Health Index began in 2016. From ensuring the continuity of care during the pandemic, to building a roadmap for recovery – what choices are leaders making, how will they change, and why?
I believe it is a leader’s job to remain strong in a crisis. During my tenure as CEO of a large university hospital in the Netherlands, I did my best to navigate through challenging times. But nothing comes close to what healthcare leaders are still facing today: the Herculean task of maintaining the same level of care for every single patient who needs it – including those for whom treatment has been delayed or cancelled due to COVID-19 – while keeping staff safe, motivated and able to do their jobs.
To say that it’s been a challenge is a huge understatement. Already under pressure from staff shortages and budget cuts, this year leaders have faced clinical, logistical and emotional hurdles of a monumental scale and scope: new waves of patients, staff burnout at all levels, extended sick leave, extra training to enable clinicians to pivot from regular units to COVID wards, and vaccination anxiety (both from the lack of jabs and concern about side effects) to name just a few. And all while coming under intense public scrutiny, some of which has been supportive, some of it less so.
In response, I know from speaking to leaders around the world that many have made bold decisions about how and where to deliver care, and where to invest in order to build resilient healthcare for the future. What I didn’t know until now is that there is a clear pattern of choices emerging among these leaders around the world.
What are those choices, and how will they change over the next few years?
This is what we wanted to uncover in our Future Health Index 2021 Report, a Philips research platform and the largest global survey of its kind [1]. We asked almost 3,000 healthcare leaders across 14 countries to tell us about how they are meeting the demands of today while preparing for a new post-pandemic reality.
Let’s look at what we’ve learned. And what’s surprising about this year’s findings.
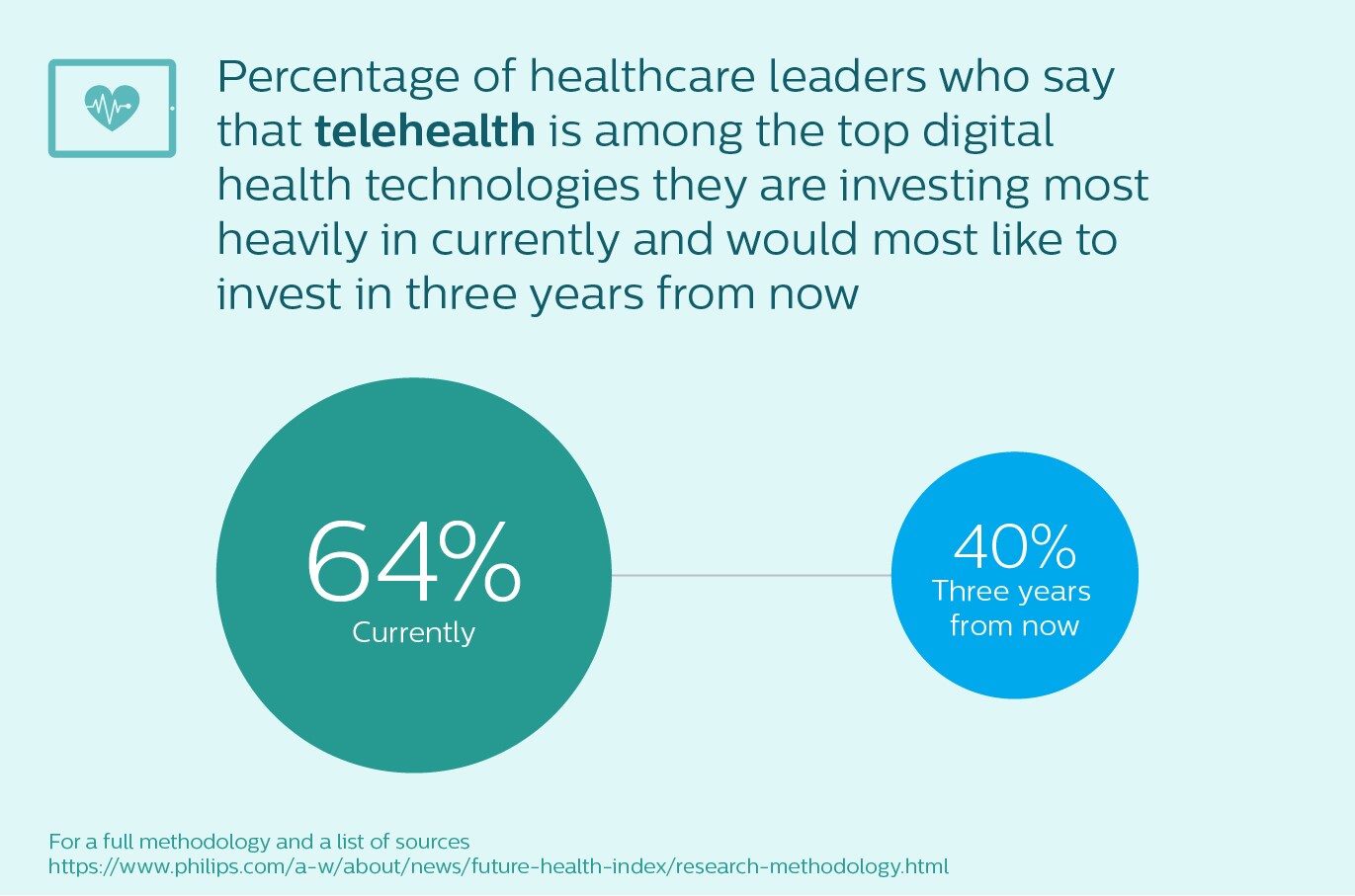
Uncertainties over the post-pandemic role of telehealth
In a year shaped by lockdowns and isolation, leaders invested heavily in virtual care to expand and extend the capacity of doctors and nurses. From screening and monitoring patients at home, to scaling up care in intensive units, we have seen many examples of telehealth gaining greater adoption since the pandemic. However, as the vaccination programs start to ease the pressure on some healthcare systems around the world, we see that their investment in telehealth solutions looks set to dip – from 64% of healthcare leaders saying that telehealth technologies are among the top digital health technologies that their hospital or healthcare facility is currently investing most heavily in, to 40% who would most like to be investing in telehealth three years from now.
I can think of three potential reasons for this: the first could simply be that the virtual care infrastructure of many healthcare facilities – and therefore the largest telehealth investment outlay – may be complete by 2024. Second, healthcare leaders may be nervous about reimbursements, which were increased for telehealth during COVID-19 but may revert to pre-pandemic levels at any point. And third, there is the simple question of whether doctors, nurses – and even patients – will have the same appetite for virtual care once the need becomes less urgent. To find out more on this topic, I can recommend this Q&A with three medical leaders at Philips.
Artificial intelligence moves past the hype
On the other hand, something that we know will become increasingly urgent is the need to deliver faster and more precise diagnosis and treatment. The toll on COVID-19 patients and their families this past year has been heavy. But with appointments delayed or cancelled, the toll on non-COVID patients over the past year has also been immense.
And it’s set to rise: research firms agree that non-COVID mortality rates and long-term mental health issues are likely to increase, as will the costs to healthcare systems; in the UK, for cancer alone, an estimated 18,000 more people will have died in the 12 months since the pandemic because of delays, which is almost 10% more than usual [2, 3, 4]. While the rapid growth in telehealth may improve access to care, it cannot entirely make up for this shortfall. Healthcare leaders urgently need to find new ways to deliver better and more efficient care.
This might explain why 40% of healthcare leaders in the Future Health Index 2021 report believe that, to be prepared for the future, implementing predictive healthcare technologies, such as artificial intelligence (AI) and machine learning, will be among the top areas their hospital or healthcare facility will need to invest in three years from now. I believe that technology cannot – and should not – replace healthcare professionals. But it can give clinicians the right information at their fingertips in the moments that truly matter.
If we take cancer diagnosis as an example, AI-enabled clinical decision support solutions can help clinicians to identify and analyze lesions on a medical image. Until recently, these types of tools were more commonly found in innovation labs rather than hospital labs. Now we’re seeing a handful of them receive the nod from organizations such as the US Food and Drug Administration [5], which leads me to expect that they will have an important impact on diagnosis and treatment in the near future.
In the six years that the Future Health Index report has been running, this year’s report is the strongest signal yet that AI is finally moving from hype to reality.

Growing recognition that strategic partnerships enable digital transformation
But healthcare leaders also reflect that they cannot do it alone. Nearly half (41%) say that their hospital or healthcare facility needs to prioritize strategic partnerships and collaborations in order to successfully implement digital health technologies. Overcoming perennial issues around interoperability and data management and stewardship looks likely to be their biggest hurdle, which is something my colleague Roy Jakobs, Head of Connected Care at Philips, will explore in his upcoming blog.

This year’s biggest surprise: sustainability
Here comes my biggest surprise. This is the first time we’ve asked healthcare leaders for their views on sustainability. I expected to see some interest, but am frankly blown away by the response we had. While understandably, the impact of COVID-19 has directed healthcare leaders’ short-term focus on immediate needs, in three years’ time the overwhelming priority of healthcare leaders in the majority of the 14 countries surveyed is to implement sustainable practices.
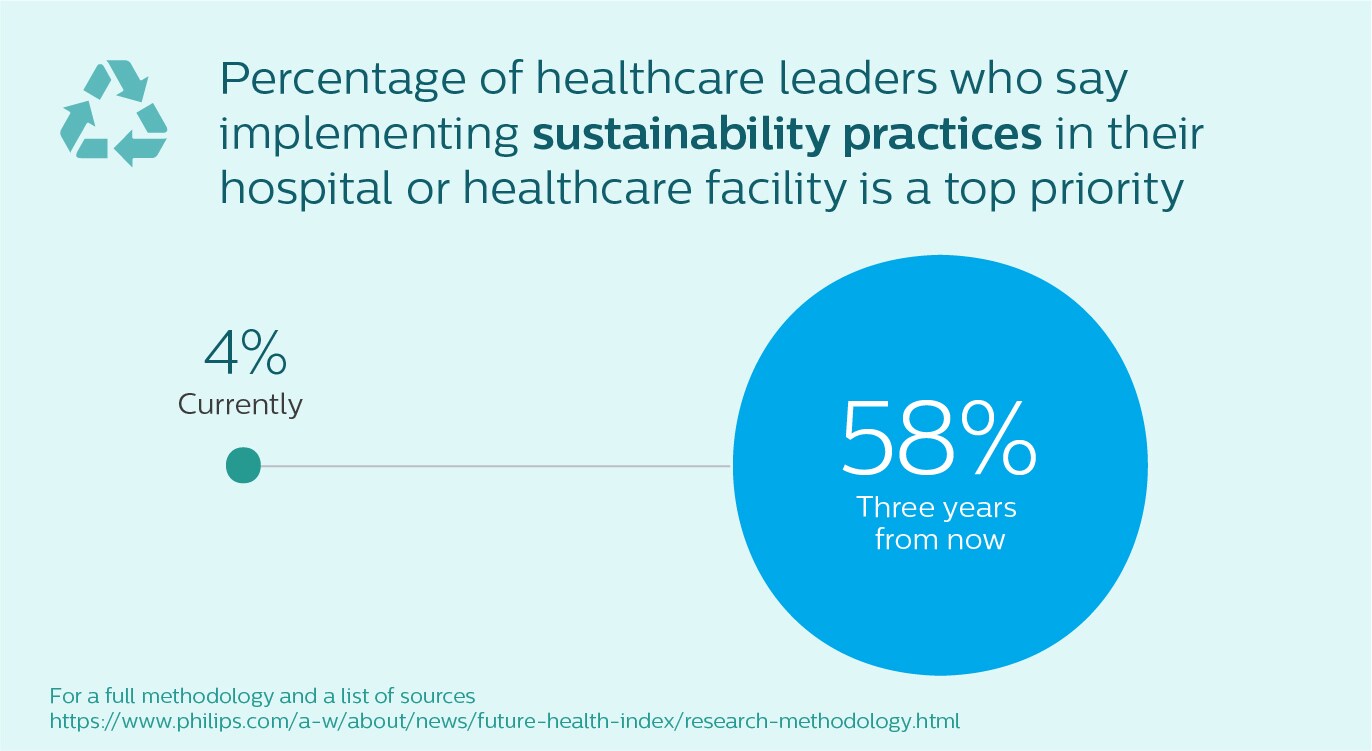
Let’s look at why this might be. In the survey, we defined sustainable practices as “environmentally conscious sourcing, recycling, etc.” The immense amount of waste created by the use of single use personal protective equipment and critical medical supplies may have encouraged healthcare leaders to reflect on the steps that they can take. Partly, I can understand it as drive for cost savings.
But I also see it as a push towards a bigger goal, where leaders no longer see sustainability practices like recycling as separate from delivering sustainable healthcare. In other words: more sustainable methods of care delivery and a strong move toward delivering better outcomes at lower cost. If you’d like to find out more about this topic, I plan to explore it in my next blog with my colleague Robert Metzke, Head of Sustainability at Philips.
I believe that resilient healthcare comes from a strong ecosystem: flexible care delivery models, motivated doctors and nurses, and decisive leaders.
Resilience comes from a strong ecosystem
A word I hear a lot these days is “resilience”. There is a collective understanding in the medical community that we need to build stronger healthcare systems that can adapt to the needs of future pandemics while continuously improving care for our growing and aging populations.
Despite the challenges leaders are still facing, it is immensely uplifting to hear from this survey that they are feeling strongly optimistic and well prepared for future; the vast majority told us that they are confident in the ability of their healthcare facility to deliver quality care three years from now (75%), and 88% are confident in the ability of their country's healthcare system to do so.
I believe that resilient healthcare comes from a strong ecosystem of flexible care delivery models, motivated doctors and nurses, and decisive leaders. And this year’s report suggests that I am not alone.
Let me be clear: we did not need the pandemic to move forward. Nevertheless, we have learned a great deal over the past year. And I believe the future of healthcare is in strong hands, crisis or no crisis.
Sources:
[1] Since 2016, Philips has conducted original research to help determine the readiness of countries to address global health challenges and build efficient and effective healthcare systems. The Future Health Index 2021 report explores the perspectives of the next generation of healthcare professionals in 14countries. For details on the Future Health Index methodology and to access the 2021 report in its entirety, visit the Future Health Index site.
[2] https://www.mckinsey.com/industries/healthcare-systems-and-services/our-insights/understanding-the-hidden-costs-of-covid-19s-potential-impact-on-us-healthcare
[3] Lai A et al., “Estimating excess mortality in people with cancer and multimorbidity in the COVID-19 emergency,” ResearchGate, April 2020, researchgate.net.
[4] https://www.cancerresearchuk.org/health-professional/cancer-statistics-for-the-uk#:~:text=Cancer%20mortality,77%2C800%20cancer%20deaths%20in%202018
[5] https://models.acrdsi.org/
Share on social media
Topics
Author

Jan Kimpen
Chief Medical Officer, Royal Philips Before joining Philips in 2016, Jan Kimpen, Professor of Pediatrics, was CEO of the University Medical Center in Utrecht. He leads the global clinical team of Philips, focusing on advocacy, customer partnerships, clinical research and medical consulting, and is responsible for the annual publication of the Philips Future Health Index. He is a strategic advisor for commercial and clinical strategy, market reimbursement, R&D roadmaps and partnerships and M&A, and provides thought leadership on relevant clinical and medical topics. Jan participates in the WEF Global Future Council on Healthcare, the American Heart Association alliance and the Board of Sanara Ventures in Israel. Jan is president of COCIR, the European trade union for imaging, healthcare informatics and radiotherapy.
Follow me on