We are all witnessing the surreal images of a society that seems to have come to a standstill with empty streets, quiet cities, deserted airports and closed bars and restaurants. At the same time, alongside the desperately sad and worrying news headlines about the spread of coronavirus, I have also read stories of immense bravery and self-sacrifice. In Wuhan, China, where nurses even shaved their heads to prevent contagion through their hair, young nurse Wu Yaling learned about the death of her mother, and minutes later went back to caring for patients. In Italy, medical student Chiara Bonini finished her final exam and headed straight for the heart of the outbreak in her hometown of Bergamo. And in the UK, 68-year old retired British doctor Alfa Saadu returned to work in London to help battle the pandemic. It’s humbling to think that there are literally millions of stories like these around the world right now. I feel incredibly grateful to every single doctor and nurse working around the clock, pushing themselves to the limit and putting their lives on the line, often with limited resources – you are the true heroes.
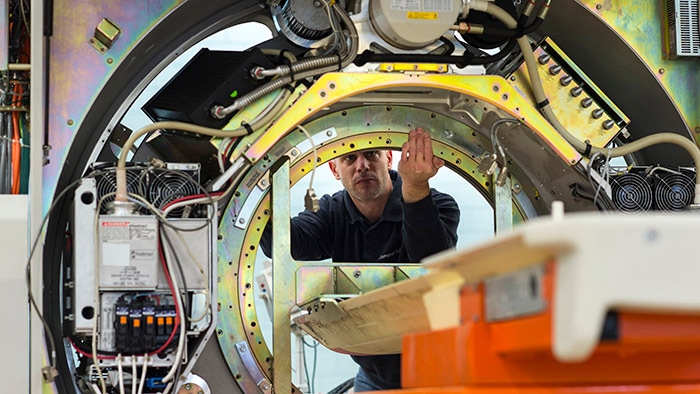
At Philips, we’re mobilizing our efforts and global resources to do what we can to support you all. I’m thinking in particular of our field service engineers who are working alongside clinicians on the front lines to keep critical care equipment in use. And also of people like Charmae Pearson, who are helping to ramp up our global production of ventilators and other medical equipment used in the diagnosis and treatment of COVID-19 patients. [1]

The demands of working in healthcare have long been immense
As both a former clinician and hospital CEO, I also wonder how this unprecedented event will change the working lives of doctors and nurses. Anyone who works in healthcare knows that clinicians across the world were struggling even before the pandemic. The 2020 Future Health Index (FHI) report, a Philips research platform [2], examined the expectations and experiences of young healthcare professionals aged under 40 and how they can be empowered to meet the demands of tomorrow’s healthcare. The results, presented in the first week of March, show that nearly three out of four younger healthcare professionals from the 15 countries surveyed experience work-related stress regularly. And more than one out of three of them have considered leaving the profession. The demands of working in healthcare have long been immense, often resulting in burnout. Hence, next to the countless personal tragedies and societal disruption that it has already caused, another possible – and also very concerning – outcome of COVID-19 could be that even more clinicians will feel frustrated by the limitations of overstretched health systems, and leave the profession for good. While that may happen, I hope and believe that many people – perhaps the young generation of healthcare professionals in particular – will be inspired by seeing how they can make an enormous difference to society and do the opposite by choosing a career in medicine. We surely need them. A recent report of the World Health Organization shows global shortfall of almost 6 million nurses. The FHI report seems to concur: the survey found that around half of those young healthcare professionals questioned feel able to drive change within their place of work.

How can we make the life of healthcare professionals easier?
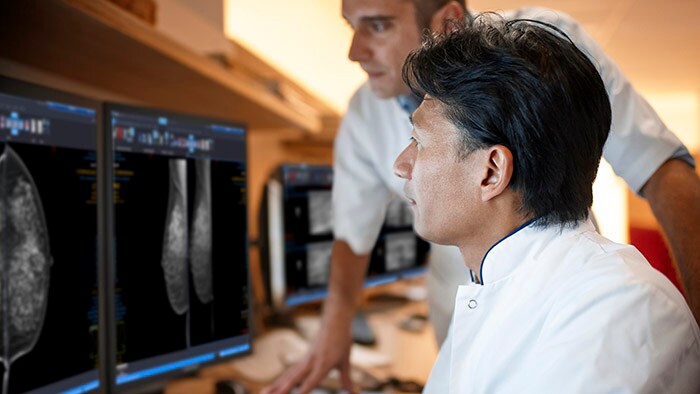
So how can we learn from this pandemic? How can we make the life of healthcare professionals easier, so that they stay in the profession, taking care of their patients, and pursuing their dreams? What would change look like in a post-COVID-19 world? I spoke recently to Professor Carlos Cordon-Cardo, Head of Pathology at Mount Sinai (US), who is convinced that things will change dramatically. For example, until recently all pathologists – who play a crucial role in the detection and diagnosis of a broad range of diseases – had to be on site in their hospital to analyze biopsy slides. But since the outbreak, the US government loosened regulations in a matter of days, enabling pathologists to read digital slides at home to review pathological cases and so prevent any delay in critical patient care. I find it hard to imagine going back to the old ways of working once we’ve seen how well clinicians can work from home. Of course, technology is not a panacea. The FHI report also lays bare the love-hate relationship that young healthcare professionals have with technology and digitization. Today’s doctors and nurses have more patients than ever, which has created a virtual avalanche of patient data. But when harnessed in the right way, I believe technology can provide enormous support.
One example is virtual care, also known as telehealth, which I addressed earlier. And in a recent blog, Jeroen Tas, the Chief Innovation Officer of Philips, discusses how online consultations are helping doctors to screen and monitor COVID-19 patients in their own homes. He also examines how critical care nurses can monitor patients in the ICU based in a remote hub using predictive analytics to prioritize patients on acuity.

Healthcare is in need of not just tweaking, but radical change
This COVID-19 pandemic has shown us how much healthcare is in need of not just tweaking, but radical change. The pressure on global health systems, providers and staff has already been increasing to unsustainable levels. But it also illustrates how much can be achieved in times of crisis: for example, both China and the UK recently built thousands of extra ICU beds in less than two weeks. I believe that healthcare reform, with a totally different approach to how healthcare is organized, delivered and distributed, will be paramount in a (hopefully soon) post-COVID-19 era. It’s the only way we can deliver on the Quadruple Aim of healthcare: better health outcomes, improved patient and staff experience, and lower cost of care.
For now, I wish everyone strength in these unsettling times. If you are one of the many who has contracted the virus, or if you have lost a loved-one, my thoughts are with you. My respect and endless gratitude goes out to everyone who is fighting the pandemic and doing what they can to help us all. At Philips, the best way we can thank our healthcare professionals is to listen to them and stay by their side, helping where we can. Now is the time to join forces, with all stakeholders, healthcare professionals, patients, governments and the private sector. And to the doctors and nurses out there like Yaling, Chiara and Alfa: You are in our thoughts, and we are forever in your debt. [1] To find out more about how Philips is helping with the global effort against COVID-19, visit our dedicated news page. [2] Since 2016, Philips has conducted original research to help determine the readiness of countries to address global health challenges and build efficient and effective healthcare systems. The 2020 FHI report explores the perspectives of the next generation of healthcare professionals in all 15 countries. For details on the Future Health Index methodology and to access the 2020 report in its entirety, visit the Future Health Index site.

Share on social media
Topics
Author

Jan Kimpen
Chief Medical Officer, Royal Philips Before joining Philips in 2016, Jan Kimpen, Professor of Pediatrics, was CEO of the University Medical Center in Utrecht. He leads the global clinical team of Philips, focusing on advocacy, customer partnerships, clinical research and medical consulting, and is responsible for the annual publication of the Philips Future Health Index. He is a strategic advisor for commercial and clinical strategy, market reimbursement, R&D roadmaps and partnerships and M&A, and provides thought leadership on relevant clinical and medical topics. Jan participates in the WEF Global Future Council on Healthcare, the American Heart Association alliance and the Board of Sanara Ventures in Israel. Jan is president of COCIR, the European trade union for imaging, healthcare informatics and radiotherapy.
Follow me on