By Alexandra Gonçalves
Cardiologist and Medical Officer for Cardiology and Personal Health, Philips
As cardiologists across the globe discover new ways of treating patients during the pandemic, one lesson is clear: COVID-19 has transformed cardiology care for the foreseeable future. Now, we must shape this transformation to benefit patients and providers long after the pandemic has ended. The future of cardiology is top-of-mind at Philips, where we work with healthcare partners to provide solutions to improve patient care and protect members of the healthcare workforce.
Adapting patient care to the pandemic
Since the pandemic started, we have been continuously learning about the relationship between COVID-19 and cardiovascular health. Early in March 2020, it became obvious that patients with cardiovascular risk factors suffer higher mortality than others with COVID-19. Later, we learned about the direct effects of COVID-19 acute illness on the heart, and just now, we are starting to understand how COVID-19 affects chronic heart disease. Equally concerning are the delays in cardiovascular care, caused by COVID-19, across the globe. Globally, 25-40% fewer patients[1] are entering the healthcare system for acute cardiovascular events. In addition, we are seeing provider partners face a backlog of so-called elective procedures, which is extremely concerning. With heart disease, what is considered elective today can lead to an emergency tomorrow.
Partnering to provide solutions
The silver lining for cardiology is that COVID-19 has accelerated the adoption of telemedicine, remote patient monitoring and diagnostic modalities that help improve patient care, such as point-of-care ultrasound and cardiac computed tomography (CT). Hopefully, these changes are here to stay. These are some of the key trends transforming cardiology during COVID-19 that should continue to improve the future of care: 1) The digitization of healthcare, including remote patient monitoring and telehealth At Philips, we have pushed to digitize healthcare long before it became part of the mainstream medical conversation. Now, our partners are seeing new value in remote patient monitoring and telehealth during the pandemic, hopefully setting the standard for digitizing care in the long term. The Philips Electronic Intensive Care Unit, or eICU, has helped healthcare workers reduce exposure to patients infected with COVID-19, while supporting them with high-quality medical expertise. The model enables teams to monitor 50–500 remote ICU beds, and has been used, so far, to monitor 4.25 million patients treated everywhere from small rural hospitals to large academic medical centers. Philips has also launched a next-generation wearable biosensor that has been used for clinical surveillance of COVID-19 patients in the hospital. For remote monitoring at home, Philips partnered with continuous health monitoring and clinical intelligence company BioIntellicence to support COVID-19 patients who don’t require hospitalization.

2) The importance of point-of-care ultrasound and cardiac CT Ultrasound has been crucial for the diagnosis of COVID-19 patients and for their evaluation throughout their hospital stay. Point-of-care ultrasound brings imaging to the patient’s bedside, providing the information needed, while limiting the risk of cross-contamination. COVID-19 has accelerated the use of point-of-care ultrasound, but the benefits of its use extend far beyond COVID-19, and are applicable to any given patient who comes into the emergency room with shortness of breath. We should expect that in the future, this becomes standard practice across the globe. As for cardiac CT, it has been found invaluable to optimize resources supporting the decision-making process regarding the need to activate the cath lab, as patients with COVID-19 myocarditis can mimic signs of acute myocardial infarction (AMI). In that scenario, healthcare providers would prepare the cath lab and clinicians involved, which requires time and personnel. Then, physicians would discover that rather than an AMI, the patient had COVID-19. Using cardiac CT, costly and unnecessary cath lab activations are being prevented and hospital admissions potentially reduced[2]. This practice is enabling better care for cardiac patients now, and expanding the role of cardiac CT for coronary artery disease assessment, which will continue beyond the pandemic.
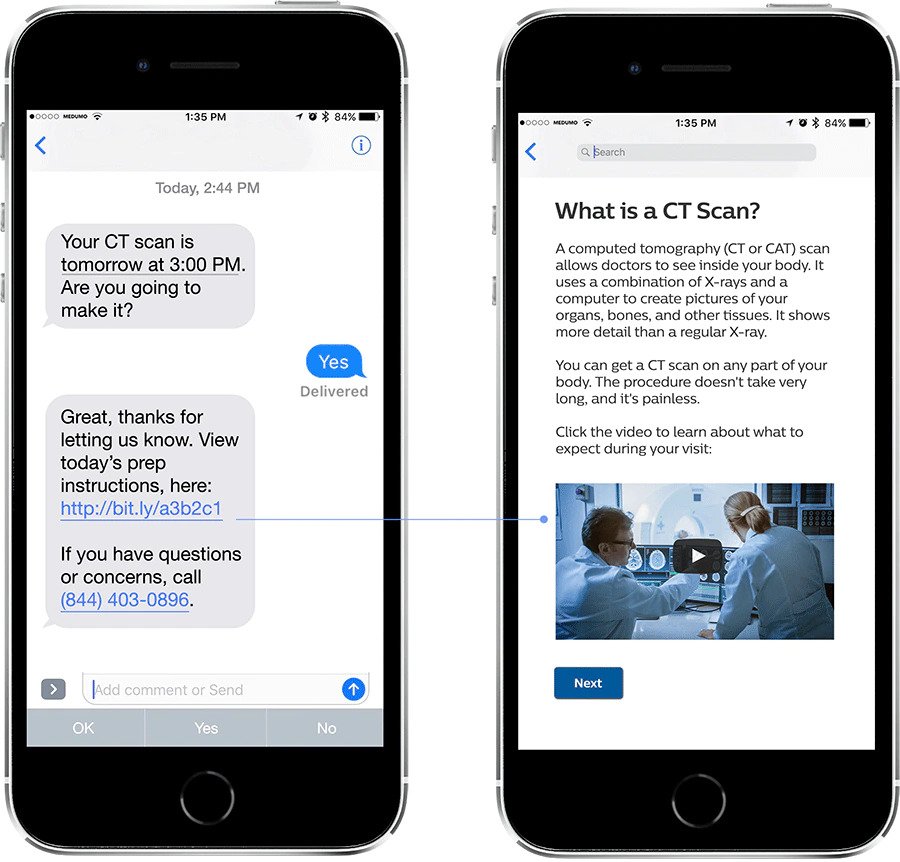
Finally, I would like to highlight the importance of trust and collaboration. Trust is fundamental to improve patient outcomes and it became even more striking during COVID. Specifically, there must be a strong link between Industry, healthcare providers and patients. During COVID-19, many providers are facing unprecedented staffing and financial challenges. Industry must be the trusted partner to provide solutions that optimize time while improving patient care and bringing the highest standards of staff safety. In addition, we must work with healthcare providers to establish trust with patients. As I mentioned earlier, many patients are delaying cardiology procedures. We need to give them confidence that they can receive the care they need while remaining protected from infection. Philips has taken a step to address the fear preventing patients from seeking treatment by empowering them with information through its Medumo platform, which helps patients prepare for their appointments, show up on time and follow specific care plans. While COVID-19 has catalyzed the implementation of patient-centric modalities and technologies in cardiology, we will only realize the full potential of this transformation if we earn patients’ trust to continue to invest in their own health. The pandemic has upended the status quo for healthcare systems, healthcare workers and patients across the world. While we adapt to the environment it has created, we must set a new standard of care for cardiology. Every patient should benefit from the innovation we have brought to the field during COVID-19, which along with trusted partnerships will certainly raise the bar for cardiology care. [1] https://twitter.com/angioplastyorg/status/1245892249101074432?s=20 [2] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7200340/ and https://pubs.rsna.org/doi/10.1148/ryct.2020200251

Share on social media
Topics
Author

Alexandra Gonçalves, MD, MMSc, PhD
Chief Medical Officer, Precision Diagnosis, Philips
Alexandra Gonçalves is Chief Medical Officer, Precision Diagnosis for Philips. Dr. Goncalves is a cardiologist with a business acumen and an extensive record of multi-disciplinary collaborations spanning the globe, as educator, author, editor, clinical researcher and though leader.
Follow me on