Enhancing TAVI efficiency: streamlining pathways for improved patient care
By Philips editorial team ∙ Dec 18, 2025 ∙ 3 min read
Faced with staffing challenges, process complexities and reimbursement changes, the Asklepios St. Georg Clinic teamed up with Philips to improve care for patients needing a Transcatheter Aortic Valve Implantation (TAVI). The result: a smoother, more coordinated experience from referral to discharge – allowing more patients to be treated while reducing hospital stays.
Case study at a glance
Partner
Asklepios St. Georg Clinic, Germany
Challenge
Growing patient demand, staff shortages, and limited coordination between departments led to high workloads, workflow inefficiencies, and avoidable delays for TAVI patients. At the same time, changes in reimbursement policies increased pressure to shorten hospital stays – a shift that research suggests may also improve clinical outcomes for TAVI patients.
Solution
Working in close collaboration with Philips, the hospital identified key areas for improvement through a multidisciplinary approach that involved all stakeholders, creating a more streamlined experience for staff and patients alike.
Results
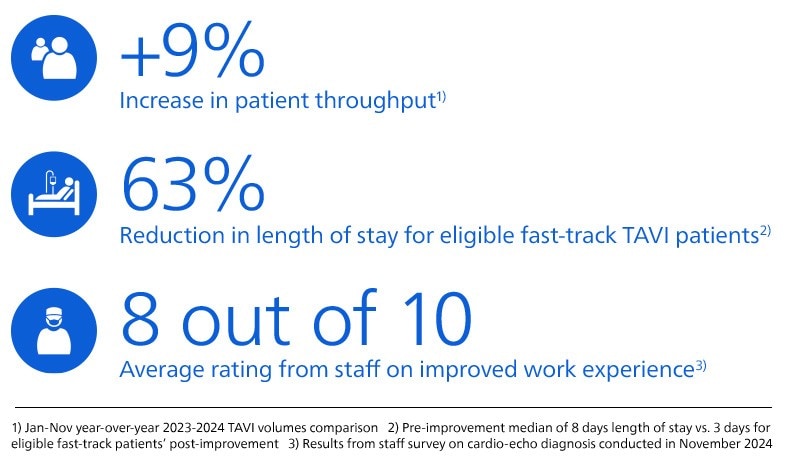
The hospital has achieved a 9% year-on-year increase in patient throughput [1] and a 63% reduction in length of stay [2] through process improvements and close collaboration across the TAVI patient pathway. Key enablers included the introduction of a fast-track protocol for eligible patients and the establishment of a centralized heart valve unit. Patient experience has also improved, supported by clear, dedicated communication and coordination of care.

In 2024, Asklepios St. Georg Clinic partnered with Philips to streamline the entire TAVI patient pathway. By taking a collaborative, multidisciplinary approach that involved all stakeholders, the hospital improved care coordination and optimized the use of available resources. Process improvements included scheduling consultations and diagnostic procedures during an ambulatory appointment up to two weeks before admission, which previously occurred after hospital admission. In addition, a ‘fast-track’ protocol enables eligible patients to follow an accelerated recovery plan, often allowing them to leave the hospital just one day after their procedure. The establishment of a central heart valve unit and enhanced communication between teams further contributed to these efficiencies. As a result, the hospital achieved significant improvements in its TAVI program, including a 9% year-on-year increase in patient throughput [1], a 63% reduction in length of stay [2] and improved staff satisfaction [3].
The challenge
TAVI (Transcatheter Aortic Valve Implantation) has revolutionized care for patients with severe aortic stenosis – turning what was once a high-risk surgical intervention into a safer, less invasive and more accessible option for a broader range of patients. As awareness of its benefits grows and populations age, demand for TAVI procedures has surged. But staffing levels haven’t always kept pace. Therefore, investing in continuous staff development was imperative to sustain quality and keep pace with growing demands.
That’s precisely the challenge Asklepios St. Georg Clinic in Hamburg faced when interventional cardiologist Dr Eike Tigges assumed responsibility for its TAVI program in 2023. “We faced a 30% reduction in capacity due to staff shortages,” he says. “We also identified inefficiencies and coordination gaps in the TAVI care pathway, placing additional strain on staff and causing avoidable delays in discharge. Multiple handoffs and ward transfers often meant patients stayed in the hospital longer than necessary. Everyone worked hard to deliver high-quality care, but without a clear vision of the full patient journey.”
This fragmented approach is echoed by Dr Da-Un Chung, who oversees all aspects of echocardiography at Asklepios – from pre-procedural assessments to post-procedural checks before discharge. “Coordinating the different patient groups we saw in our clinic – not just TAVI patients but also other types of patients – was challenging,” he says. “All patients had to go through the same echocardiography lab with limited staffing, which sometimes led to long waiting times for patients. We saw similar bottlenecks with postprocedural scans before discharge.”
As a result, TAVI patients stayed in the hospital for an average of nine days. While this was in line with the national average in Germany, Dr Tigges believed his team could do better. “Research suggests that earlier discharge benefits patients,” he explains. “It lowers the risk of infection and helps speed up recovery. And we know that for most patients, it’s safe to go home sooner.”
Upcoming hospital reforms and reimbursement changes in Germany have created additional pressure to optimize productivity and increase patient throughput, Dr Chung adds. “With new regulations determining which hospitals can continue performing certain procedures – and how many – we realized we needed to strengthen our TAVI program to deliver the best possible care and treat more patients, while ensuring an optimal length of stay in the hospital.”
The solution
Faced with these challenges, Asklepios undertook a comprehensive restructuring of its structural heart program. This included a team-centered approach with clearly defined structures and a KPI-based review process – fostering transparency, supporting staff development, and aligning efforts toward shared goals.
As a key part of this transformation, Asklepios partnered with Philips to help optimize the entire TAVI patient pathway, strengthen collaboration, improve efficiency, and enhance patient satisfaction. Dr Tigges: “Our goal was to perform 500 TAVI procedures annually by 2025, up from 463 in 2024 and 399 in 2023. We also aimed to reduce the length of stay to three days where possible – maintaining quality of care with the same staffing levels but at a lower workload, while allowing patients to return home sooner.”
Taking a co-creation approach with all stakeholders
To deliver on these ambitions, Asklepios and Philips worked together to identify key areas for improvement through a collaborative, multidisciplinary approach.
“We wanted to improve the entire patient pathway, from referral to discharge, and that meant bringing together everyone who plays a role in TAVI care,” says Dr Tigges. “Real change doesn’t happen in isolation – it takes inputand collaboration across all roles and departments.”
“By involving everyone from nurses to care planners, we looked for improvements that would work for our colleagues delivering care, as well as the patients receiving it,” he continues. “Teaming up with Philips also gave us afresh perspective. It challenged us to rethink the way we’d always done things.”
The collaboration with Philips started by framing the current state through onsite observations, interviews and workflow mapping. Through collaborative workshops, the team identified targeted improvements and developed action plans across the entire patient pathway.

We wanted to improve the entire patient pathway, from referral to discharge, and that meant bringing in everyone who plays a role in TAVI care. Teaming up with Philips also gave us a fresh perspective. It challenged us to rethink the way we’d always done things.
Introducing a dedicated heart valve unit and fast-track protocol
One of the main improvements that the Asklepios team developed in collaboration with Philips was the creation of a separate heart valve unit. This unit centralizes patient care for TAVI patients and helps expedite both diagnostic and discharge processes.
“Having a dedicated heart valve unit helps us guide patients much more efficiently based on the type of exam they need,” Dr Chung explains. “It means the right nurse is there at the right time for the right patient, so we cut down on wait times and reduce the need for constant back-and-forth among staff.”
Asklepios also introduced a ‘fast-track’ protocol for TAVI patients who are considered low-risk based on a thorough pre-procedural health assessment. Consultations and diagnostic procedures that used to happen after hospital admission are now scheduled during an ambulatory appointment up to two weeks before admission. The fast-track protocol also allows eligible patients to follow an accelerated recovery plan, often leaving the hospital just one day after their procedure. “We realized earlier discharge was possible for some patients, and now we have a process in place to make it happen,” says Dr Chung.

We realized earlier discharge was possible for some patients, and now we have a process in place to make it happen.
Streamlining collaboration and communication at every step
At the heart of the optimized ways of working are Kristina Veltrup and Anna-Lena Fink, the hospital’s dedicated TAVI coordinators. Their newly created roles help ensure each patient’s journey runs as smoothly as possible, with minimal delays throughout.
“One of the biggest issues in the past was communication,” says Ms Fink. “There were gaps between nurses and doctors, and between staff and patients. As a result, people often had incomplete or inconsistent information or simply didn’t know what was happening with the patient.”
To address this fragmentation, every step of the patient journey was carefully mapped and redesigned – through workshops facilitated by Philips – to enhance collaboration and efficiency.
Ms Veltrup manages the pre-procedural phase of the patient journey, overseeing referrals, planning, scheduling and heart team meetings. She explains, “It’s all about making sure everything is in place at the right time, so the process runs smoothly. I coordinate with all involved parties, including referrers, ward doctors, nurses, cardiologists and surgeons.”
Meanwhile, Ms Fink focuses on the post-procedural aspects, including discharge and coordination with social services. “Being based on the heart valve unit means I see patients soon after surgery,” she says. “I answer their questions and help facilitate the transition to home care. It has helped shorten hospital stays and made it easier for patients to know who to turn to, especially when doctors or nurses aren’t immediately available. And because I work closely with social services, we can coordinate follow-up care more quickly and efficiently.”

Having a dedicated coordinator has helped shorten hospital stays and made it easier for patients to know who to turn to, especially when doctors or nurses aren’t immediately available.
The results
Thanks to the close collaboration across teams, Asklepios achieved all its goals with the newly optimized TAVI patient pathway: more patients treated, shorter hospital stays and greater staff satisfaction through improved planning and communication.
“We are now able to perform an average of seven TAVI procedures per day – more than double our previous capacity of three – allowing us to treat four more patients daily,” says Dr Tigges. “And thanks to the fast-track protocol, we’ve cut the median stay for eligible patients from eight days to just three. That frees up beds sooner and helps us care for more patients without compromising on quality – keeping us well on track to reach 500 procedures in 2025.”
Staff satisfaction is up as well: a survey among echocardiography staff showed an average rating of 8 out of 10 for improved work experience. Ms Veltrup: “The biggest difference is that there’s now a clear structure for everyone, which covers the entire patient journey – from admission to discharge – so nothing gets lost along the way. Doctors appreciate that they can call me anytime, and that I know what’s going on.”
Patients have also responded positively to the process improvements, Ms Fink adds. “I follow up with fast-track discharged patients two weeks after their procedure to ask how they are doing and to check for complications. So far, we’ve only received positive feedback. Patients know they can reach out to us at any time if they need support. Referring physicians also benefit from centralized communication, with direct access to our team.”
For Ms Veltrup, stepping back from day-to-day work was key to driving improvements. “In the clinic, we rarely have time to reflect on how to do things better because we’re focused on patient care. The workshops with Philips offered us valuable time to rethink our approach with external guidance. I felt that everyone, including the doctors, really listened to our ideas and took us seriously. That close connection with doctors is also what makesworking at Asklepios special for me.”
This sentiment is shared by Dr Timm Ubben, senior consultant cardiology at Asklepios, who was closely involved in the process mapping and improvements. “The work with Philips has helped everyone understand how their roles interconnect, creating a shared focus on the patient. It brought us closer together, knowing we’re all working toward the same goal.”
Looking ahead, Dr Chung concludes: “Of course, there’s always room for further improvements, but we’re already seeing interest from other parts of the hospital wanting to learn from our approach.” Dr Tigges adds: “Building on the success of our program, Asklepios has decided to establish a dedicated division for structural heart interventions. It’s a clear sign of the strong positive impact this project has had – and its potential to inspire further change.”

The work with Philips has helped everyone understand how their roles interconnect, creating a shared focus on the patient. It brought us closer together, knowing we’re all working toward the same goal.
Sources
[1] Jan-Nov year-over-year 2023-2024 TAVI volumes comparison [2] Pre-improvement median of 8 days length of stay vs. 3 days for eligible fast-track patients’ post-improvement [3] Results from staff survey on cardio-echo diagnosis conducted in November 2024







